Imagine, Surgery Without a Scar
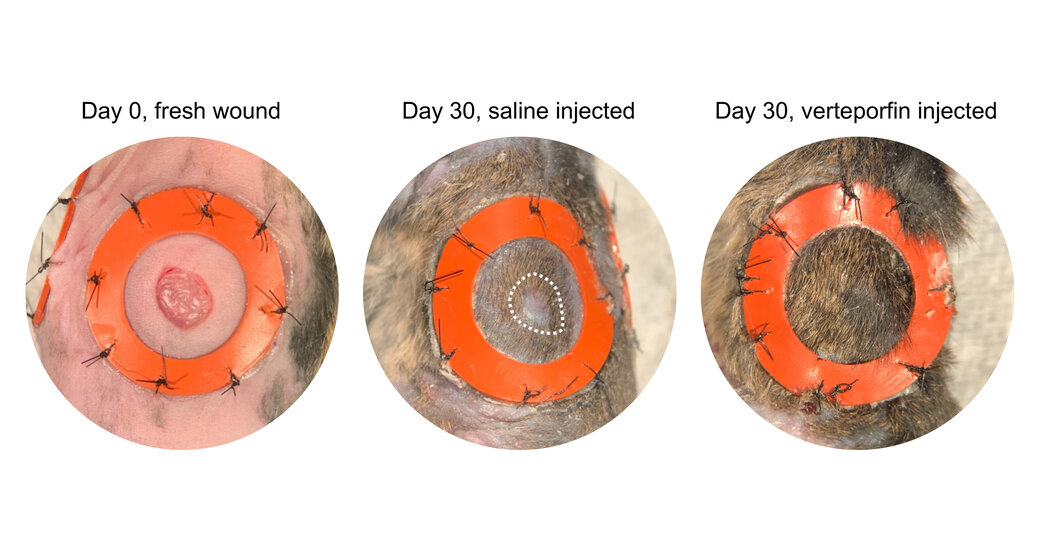
A new study shows that a 20-year-old drug prevents scarring in mice. If it works on humans, it could change the lives of those with disfiguring wounds.Cleft palates that close without scars. Burn wounds that recover without a trace of injury. Years-old disfiguring scars that disappear, leaving skin smooth and flawless.It sounds like science fiction, but healing without scarring may become a tantalizing possibility. In a study published Thursday in Science, two researchers at Stanford University report that they have figured out the molecular signals that make scars form and found a simple way to block them — at least in mice.A 20-year-old drug, verteporfin, already on the market as an intravenous treatment for macular degeneration, can prevent scarring if it is injected at the edge of a wound.As the verteporfin-treated wounds heal, the skin that forms looks perfectly normal, nothing like skin that heals with scars, those lumpy wound closures that are not only unsightly but also much weaker than normal skin and have no hair, or oil and sweat glands.The study involved mice, but the researchers, Dr. Michael Longaker, Stanford’s vice chair of surgery, and Geoffrey Gurtner, Stanford’s vice president of surgery for innovation, have now moved on to pigs, whose skin is closest to that of humans. With these new subjects, the surgeons made an incision as wide as a thumb and five inches long. When they sutured the cut and injected verteporfin around the edge, there was dramatically less scarring.“It’s pretty spectacular,” Dr. Longaker said.Researchers who study wounds and who were not associated with the study were enthusiastic.“It is unusual for me to read a paper and say, ‘Wow, this is really a major advance,’” said Valerie Horsley, a tissue developmental biologist at Yale who studies wound healing. “But this is a major advance.”Marjana Tomic-Canic, director of the wound healing and regenerative medicine program at the University of Miami Miller School of Medicine, said that the study is “really a leap,” adding, “everyone will get excited about this work.”Dr. Longaker said that he hoped to get permission from the Food and Drug Administration by the end of the year to test the safety and efficacy of the drug in babies with cleft lips and palates.For Dr. Longaker, speed is of the essence if the treatment works and is safe. “I don’t want this to be a 10-year journey,” he said.Stanford has filed patents for the use of verteporfin in scar formation.Although verteporfin is available, and doctors can prescribe drugs for unapproved uses, Dr. Longaker says that it’s crucial to wait for F.D.A. approval before using the drug to try to prevent scars.“Obviously we want to help patients as soon as possible,” he said. “But we’ve got to make sure this drug is tested in a way that ensures safety and efficacy.”The history of medicine, he said, offers a sobering picture of treatments that looked good in animals but failed in clinical trials.If the drug works on humans, the discovery stands to be lucrative and life transforming. Hundreds of millions of people are seriously scarred each year, and many of those scars are disfiguring — from accidents, as well as from heart bypass surgeries, mastectomies and burns.“Scars in general cause pain and itching and prevent us from moving the way we should,” said Dr. Benjamin Levi, a burn specialist who directs the Center for Organogenesis and Trauma at the University of Texas Southwestern Medical Center. The possibility of blocking the scarring process “has huge potential,” he said.Dr. Jason A. Spector, professor of plastic surgery and otolaryngology at Weill Cornell Medical College, said that when he does reconstructive surgery on patients with head and neck cancer, many “are more concerned about the scar through their lip and skin than about the cancer itself.”Dr. Longaker’s obsession with scars began with an experiment in 1987 as a new postdoctoral fellow in the lab of Dr. Michael R. Harrison at the University of California, San Francisco. Dr. Harrison, who was studying fetal surgery, suggested that Dr. Longaker operate on a fetal lamb two-thirds of the way through pregnancy and then return the fetus to its mother’s womb to continue developing.Dr. Longaker gasped when he later delivered the baby lamb. Its skin was intact. There were no scars to be seen.“I will never forget that moment,” he said.He went on to become a pediatric plastic surgeon and saw firsthand the scarring on children after they had undergone operations for cleft lips or palates. And he ran a lab devoted to figuring out how to prevent scars.He learned that for the first two trimesters of fetal life, skin is gelatinous, “like a bowl of Jell-O,” Dr. Longaker said. Then, as the fetus develops to live outside the sterile liquid world of the womb, the skin forms a barrier to prevent water loss and block the entry of microorganisms. At that point, breach of the skin barrier could be deadly, so the body switches on a system that lets it quickly seal it.But there is a trade-off for speed in healing a wound, Dr. Longaker noted. “The cost is loss of form and function.” And scar formation.Dr. Tomic-Canic described the process: When there is a wound, the strong muscle under the skin contracts and brings the edges of the wound together. A clot forms as a temporary barrier over the wound, and under it, the body makes thick coils of collagen rope that form a bridge so skin cells can migrate across the gap and fill in the opening. Those collagen ropes remain — they are the scar.As molecular biology and molecular genetics advanced, Dr. Longaker seized on the new tools to probe the molecular pathways needed to form scars. The key starting point for scarring is mechanical tension when a wound tears skin that should be taut. (Older people with loose skin are less likely to scar because their skin is under less tension.) The tear in the layers of skin prompts a type of skin cell — fibroblasts — to create collagen ropes and initiates a chain reaction of molecular events inside the skin cells. The reactions culminate in the activation of a protein called YAP, for Yes-associated protein. YAP then binds to DNA, and scarring begins.Dr. Longaker and Dr. Gurtner bred mice without the YAP protein. Because mice have loose skin, the two had to hold the wounds open with a ring, like an embroidery hoop, to mimic the tension in human skin. The wounds healed. No scars.They then asked: Could verteporfin have the same effect as the absence of YAP? So in another experiment, they wounded mice that could make YAP and once again held the loose skin taut with rings. They injected verteporfin around the wound. They waited to see what would happen.Dr. Longaker remembers the moment. “Holy guacamole,” he said. The healed wounds looked just like normal skin. They were the same under the microscope. They grew hair. They had oil glands.His imagination soared. He might be able to prevent scars with a few quick injections of verteporfin. And there was no reason to think he couldn’t go even farther. A patient who had a disabling and disfiguring scar could go to a surgeon who could dab the scar with lidocaine to numb the skin, cut open the scar, inject verteporfin around the edges, and close the wound. Would it reheal without the scar?“That could change their lives,” Dr. Longaker said.Dr. Spector said he doubted all doctors would wait until F.D.A. approval if early clinical data supported the laboratory studies. Some are sure to jump ahead and try it because there is nothing now to stop scarring.Dr. Longaker hopes doctors hold off. Clinical trials must come first, he stressed, and safety must be assured.“I get it,” he said. “No one is more excited than me.”“To be honest,” he added, “I’ve been waiting for 34 years. I would love to use it. This is a big deal. But that doesn’t mean we shortcut the process.”
Read more →