India Covid: The messages deciding between life and death
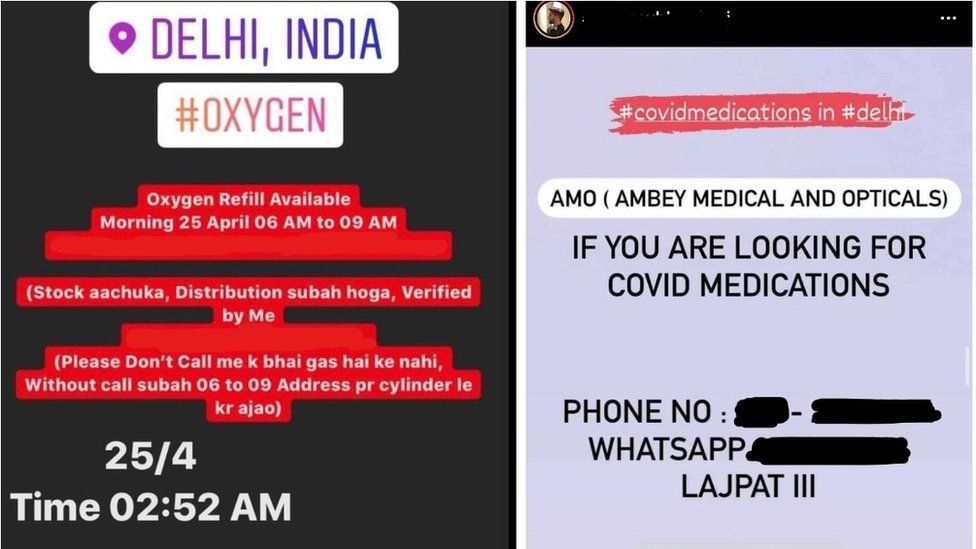
SharecloseShare pageCopy linkAbout sharingimage copyrightInstagramAs a second wave of coronavirus devastates India, with more than 350,000 cases reported daily, the families of the sick are desperately hunting on social media for help. From morning to night, they scour Instagram accounts, drop messages on WhatsApp groups and work through their phone books. They’re looking for hospitals beds, oxygen, the Covid drug Remdesivir and plasma.It’s chaotic and overwhelming. A WhatsApp message starts circulating: “Two ICU beds free.” Minutes later, they’re gone, to be occupied by whoever got there first. Another message: “Urgently needed oxygen concentrator. Please help.”As the health system buckles, it is community, self-help and luck standing between life and death. But demand is outstripping supply and the sick don’t have the luxury of time. When I started this piece on Friday, I spoke to one man looking for oxygen on WhatsApp for his 30-year-old cousin in Uttar Pradesh. By the time I finished it on Sunday, he had died.Others are exhausted and distressed after days of shouldering the weight of finding life-saving treatment for their loved ones.”It’s 6am in India and that’s when we start the calls. We find out my grandpa’s needs for the day – oxygen or injections – and we hit WhatsApp and we call everyone we know,” Avani Singh explains.image copyrightAvani SinghHer 94-year-old grandfather is extremely ill with Covid-19 in Delhi. From their home in the US, Avani and her mother, Amrita, describe a dizzying web of family, friends, relatives and professional contacts, sometimes many times removed, who helped when he fell ill and quickly deteriorated.”We were working every contact we know. I was looking on social media – there are pages I follow that say ‘so and so confirmed has ICU beds’ or ‘this place has oxygen’ – between us we tried around 200 places,” Avani explains.Eventually through a school friend they found a hospital with beds but discovered it had no oxygen. By now, Avani’s grandfather was unconscious. “Then I posted a plea on Facebook and a friend knew an emergency room with oxygen – because of that friend my dad survived the night,” Amrita explains.Read more of our coronavirus coverage:Why India’s second coronavirus wave is devastatingPatients suffer at home as Covid chokes hospitalsThe viral picture that defines India’s Covid distressWhy India is running out of oxygen againWhen we speak on Saturday, his outlook has improved but the task ahead for Avani and Amrita is to get hold of Remdesivir injections. They make the calls and Amrita’s brother in Delhi drives to the locations, clocking up to a 100 miles (160km) a day. “My grandad is my best friend. I can’t thank the people running the Instagram pages enough for everything they are doing,” Avani says.But information quickly goes out-of-date and they’re worried about fakes.”We heard one pharmacy had them, but by the time my cousin got there, there was none left. It opened at 8.30am and people had been queuing from midnight – only the first 100 got the injections.”Now they are selling medicine on the black market – it should be 1,200 rupees ($16) and they’re selling for 100,000 ($1,334) – and you can’t guarantee it’s real,” Amrita explains.And like in any system that relies on personal connections, not everyone has a fair shot. Money, family contacts and a higher social status all bring a greater chance of success, as does access to internet and mobile phones.Amid the chaos, individuals are pitching in to try to bring some order and centralise information, setting up community groups and using Instagram accounts to circulate contacts.Arpita Chowdhury, 20, and a group of students at her college in India’s capital, Delhi, are running an online database of information they gather and verify themselves. image copyrightArpita Chowdhury “It’s changing every hour and minute. Five minutes ago, I was told that there is a hospital with 10 beds available, but when I call there are no beds available,” she explains.With her colleagues, she calls contact numbers advertised on social media that offer oxygen, beds, plasma or medicine and publishes the verified information online. She then fields requests from relatives of Covid patients asking for help.”At the most basic level, it’s something we can do to help,” she says.On Friday, Aditya Gupta told me he was searching for an oxygen concentrator for his dangerously-ill cousin Saurabh Gupta in Gorakhpur, a town in the northern state of Uttar Pradesh, which has been reeling from a rising cases and deaths. image copyrightAditya GuptaSaurabh, a 30-year-old engineer, was his family’s pride and joy. His father ran a small shop and had saved up so he could get an education.”We visited almost all hospitals in Gorakhpur. The large hospitals were full and the rest told us: ‘If you can arrange oxygen on your own, than we can take the patient,” Aditya explained.Through WhatsApp, the family got hold of one oxygen cylinder but needed a concentrator to make it work. It was out-of-stock on Friday but they received assurances from a supplier that they could get one.But the desperately needed device never arrived and Saurabh was never admitted to hospital.On Sunday Aditya explained: “We lost him yesterday morning, he died in front of his parents.”
Read more →