Louise Levy, Who Was Studied for Her Very Long Life, Is Dead at 112
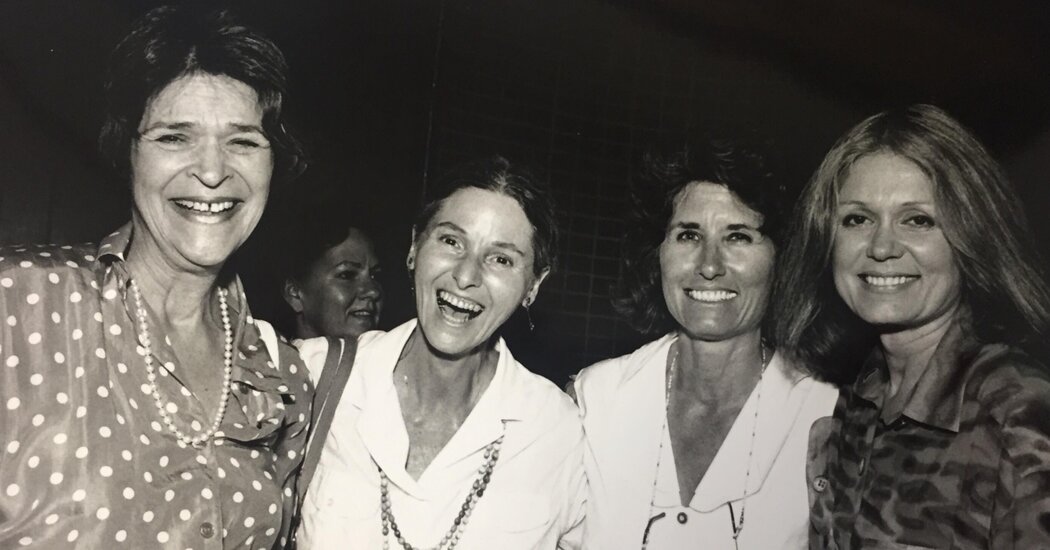
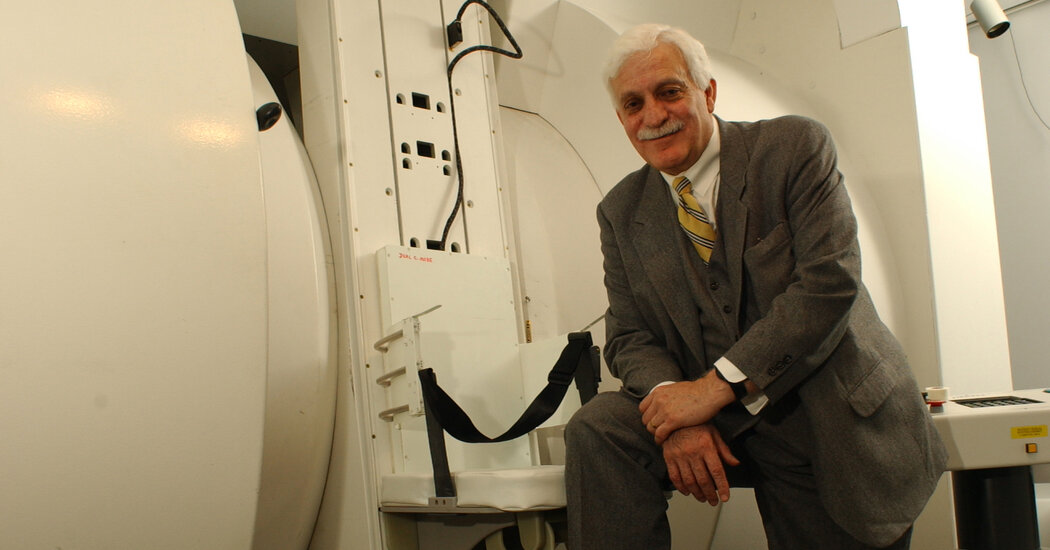
She was one of hundreds of people, all of them Ashkenazi Jews, whose good health and cognitive ability at extreme old age were the subject of genetic research.Louise Levy, who along with hundreds of others 95 and older was part of study to understand how their genetic makeup led to their good physical and cognitive health during extremely long lives, died on July 17 in Greenwich, Conn. She was 112.Her daughter, Lynn Neidorf, confirmed the death, at a hospital. She said Mrs. Levy had broken a hip two months ago but, after surgery and rehabilitation that had her moving with a walker, had developed an infection that weakened her.At her death she was one of the world’s six living supercentenarians, people who have lived into a 12th decade, according to the Los Angeles-based Gerontology Research Group.“She was a light of positivity,” Ms. Neidorf, who is in her 70s, said by phone. “She had that quality babies have: People were drawn to her. They wanted to be around her.”Mrs. Levy lived independently in a senior living community in Rye, N.Y, until two years ago, during the pandemic, when she moved into its assisted living facility.When she celebrated her birthday last year, she told The Rye Record, “I’m glad I can still speak and have my sense of humor, but I would caution you not to try and live to be 112!”She had been the oldest known living person in New York State, according to LongeviQuest, which maintains a database of supercentenarians.Mrs. Levy was one of more than 700 people, all 95 or older, recruited since 1998 to participate in a study by the Institute for Aging Research at the Albert Einstein School of Medicine in the Bronx to learn the genetic reasons for their unusually long, healthy lives.“It’s not luck,” Dr. Nir Barzilai, an endocrinologist who directs the institute, said by phone. “They exceeded luck. The biggest answer is genetics.”Using the blood and plasma of the test group, all Ashkenazi Jews — a comparatively homogeneous population whose genetic variations are easier to spot — the institute’s Longevity Genes Project has discovered gene mutations that are believed to be responsible for slowing the impact of aging on people like Mrs. Levy and protecting them against high cholesterol, heart disease, diabetes and Alzheimer’s disease.“The most striking thing about them is they had a contraction of morbidity,” Dr. Barzilai said. “They are sick, as a group, for very little time at the end of their lives.”He added, “Did they do what we know we should do — exercise, diet and sleep and have social connectivity? The answer is mostly no. Sixty percent were smoking. Less than 50 percent did much household activity or biking. Fifty percent were overweight or obese. Less than three percent were vegetarians. So they weren’t special in that sense.”The goal of the research is the development of drugs that would imitate what the centenarians’ genes do to protect their health.Louise Morris Wilk was born on Nov. 1, 1910, in Cleveland. Her father, Louis, was a photographer and a movie theater manager. Her mother, Mollie (Morris) Wilk, was a homemaker. The three later moved to New York City, where Louis illustrated film posters.Louise in 1918, not long before the end of World War I.via Levy FamilyLouise attended but did not graduate from Hunter College. In 1939, she married Seymour Levy, who sold housewares for a company founded by his father. He later took over the company, and Mrs. Levy became his office manager when he moved the business into their house in Larchmont, N.Y.She continued to work into her 90s for the man who acquired the company after her husband died in 1991.“Not full time, you know — two, three days a week for an hour or two until my car conked out,” she told WCBS Radio in 2019.Mrs. Levy did not have heart disease, diabetes or Alzheimer’s disease but was treated for breast cancer and smoked cigarettes for decades, until 1965, when the U.S. Surgeon General put health warnings on cigarette packs.Even as her hearing, eyesight and mobility diminished, she stayed active with stretching classes, playing bridge and knitting sweaters for hospitalized babies. She began losing her short-term memory only in the last six months.Mrs. Levy believed that her low-cholesterol diet, positive attitude and daily glass of red wine contributed to her extended good health. “Everybody says ‘good genes,’” she told the Canadian newspaper The National Post in 2012, “but I don’t think it’s good genes.”She may have been onto something.“There is more than one way to get to 100,” Dr. Barzilai said, “but some of them are genes that are related to cholesterol.”In addition to her daughter, Mrs. Levy is survived by her son, Ralph, who is also in his 70s, four grandchildren and six great-grandchildren.Ms. Neidorf, who believes her own good health may be tied to the same genetic makeup as her mother’s, recalled that the two were nonetheless different types of people.“I was much more fresh and disobedient than she was,” Ms. Neidorf recalled. “She was sugar and spice and everything nice. I held her in great admiration because she never tried to make me be like her. She accepted who I was and believed in me.”
Read more →