Inside a Campaign to Get Medicare Coverage for a New Alzheimer’s Drug
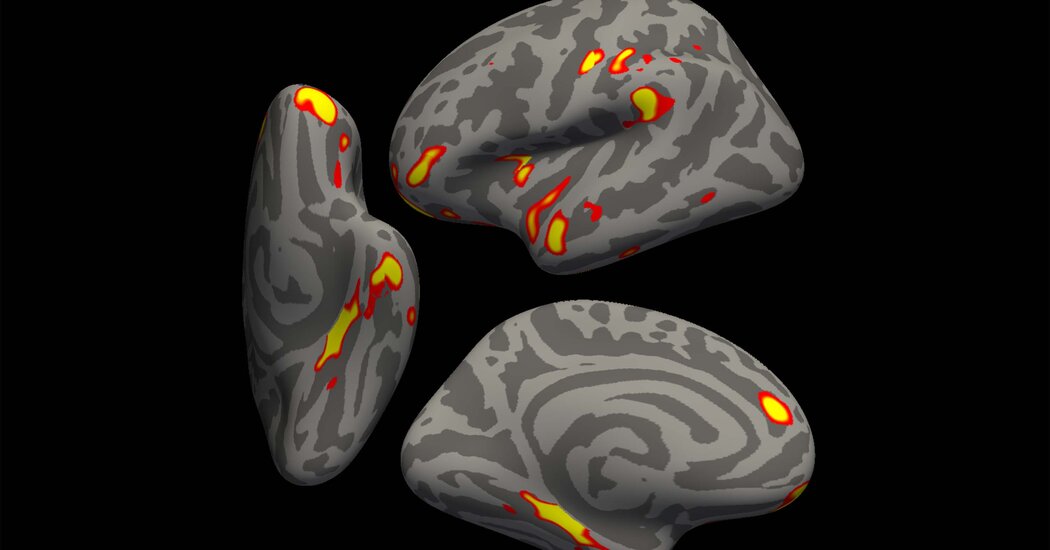
The Alzheimer’s Association has pushed relentlessly to get broad access to Aduhelm, despite safety risks and uncertain evidence that it helps patients.The day after Medicare officials announced a preliminary decision to sharply limit coverage of the controversial new Alzheimer’s medication Aduhelm, citing its unclear benefit and serious safety risks, the nation’s most prominent Alzheimer’s advocacy organization convened its policy team.The agenda: fighting Medicare’s proposal.“This is our top priority,” Robert Egge, the association’s chief public policy officer, said at the Jan. 12 session, according to recordings obtained by The New York Times.The next day, the chief executive, Harry Johns, took the mission to the entire staff, saying, “You can count on us being relentless.”Medicare’s proposal to pay for Aduhelm only for participants in randomized clinical trials was welcomed by many Alzheimer’s experts and other doctors. They say it would protect patients and families whose desperation might lead them to try anything, while also rigorously evaluating whether Aduhelm actually works.But the Alzheimer’s Association and similar groups, along with Aduhelm’s manufacturer, Biogen, strongly object. They say that Aduhelm, a monoclonal antibody that is the first drug approved for Alzheimer’s in 18 years, should be covered for anyone with mild Alzheimer’s-related cognitive decline and that usage decisions should rest with patients and their doctors.The association’s campaign makes little mention of Aduhelm’s safety risks and uncertain benefit, arguing that restricting coverage of an F.D.A.-approved drug is “shocking discrimination against everyone with Alzheimer’s disease.”With Medicare’s final decision due by April 11, the group has organized tweets directed at President Biden, emails directed at Congress, and ads on social media and websites including Univision, Essence and Martha Stewart.It has orchestrated over 400 meetings in which people with Alzheimer’s, their family members or supporters have implored their members of Congress to press the Centers for Medicare and Medicaid Services (C.M.S.) to broadly cover the drug. In sessions prepping for those meetings, association officials suggested that people say versions of phrases like “I have a fatal disease and I want more time with my family” and to discuss “how access to F.D.A.-approved treatments will impact me and my family.”Leaders also encouraged people to submit comments to C.M.S. in ways that weren’t scripted. “It is important that individuals not use our talking points,” Beth McMullen, senior director of grassroots advocacy, instructed at one meeting. Employees filing comments “cannot submit as a staff member of the Alzheimer’s Association,” she said.The push reflects growing activism by advocacy groups involved in various diseases, which sometimes campaign for therapies despite medical experts’ concerns about insufficient data. Some are partially funded by pharmaceutical companies. In fiscal year 2021, the Alzheimer’s Association received $1.6 million from manufacturers developing monoclonal antibodies, including $487,500 from Biogen.Biogen, Aduhelm’s manufacturer, gave the Alzheimer’s Association $487,500 in fiscal year 2021.C.J. Gunther/EPA, via ShutterstockOther Alzheimer’s advocacy groups are also campaigning, including UsAgainstAlzheimer’s. It has run television ads featuring patients and has written in strident language to C.M.S. that “the government would be consigning millions of Americans to inevitable decline and death, with no possibility of appeal.” The Alliance for Aging Research led a rally of about 100 people outside the Department of Health and Human Services, which houses C.M.S. (Afterward, about half the alliance’s scientific advisory board quit in opposition to the group’s position.)Understand the New Alzheimer’s Drug AduhelmF.D.A. Approval: The agency approved the first new Alzheimer’s treatment in 18 years despite fierce debate over whether it works.Potential Safety Risks: Concerns over Aduhelm intensified after a 75-year-old woman in a clinical trial developed brain swelling and died.Medicare Limits: Officials said the federal program should cover the drug only for patients who are participating in approved clinical trials.Understand Alzheimer’s: Get answers to common questions about the disease, which affects about 30 million people globally.Medicare’s coverage proposal came after Aduhelm, an expensive monthly infusion that also has the scientific name aducanumab, was approved in June by the Food and Drug Administration despite contradictory scientific results. Participants in one clinical trial appeared to experience slight slowing of cognitive decline, while patients in a nearly identical trial didn’t appear to benefit at all. About 40 percent of patients on the dosage later approved experienced brain swelling or brain bleeding, often mild, but sometimes serious. Both a council of senior F.D.A. officials and the agency’s independent advisory committee had said there wasn’t enough evidence for approval. Questions about the approval, and whether the F.D.A. worked too closely with Biogen, have prompted investigations by congressional committees, the Health and Human Services department’s inspector general, the Federal Trade Commission and the Securities and Exchange Commission. Major medical centers, including the Cleveland Clinic, have declined to offer Aduhelm.After C.M.S. announced its proposal, Dr. Lee Fleisher, the agency’s chief medical officer, said, “Our foremost goal is to protect beneficiaries from potential harm from an intervention without known benefits in the Medicare population.”The proposal has attracted extraordinary interest, with C.M.S. receiving 9,957 comments, some organized by advocacy groups on both sides of the debate.The Alzheimer’s Association, with revenue of about $400 million, is highly influential in the Alzheimer’s field: It runs an international conference, provides research grants and publishes a journal.In recordings of the staff meeting and two prep sessions, association officials didn’t mention Aduhelm’s safety risks.In an interview, Mr. Johns, the chief executive, said, “We take the safety concerns seriously,” adding, “The risks are real, but they’re not worse than treatments that are covered by Medicare today.” He proposed that patients enroll in a registry where negative effects could be reported. But many experts say that wouldn’t sufficiently evaluate the drug. At the staff meeting, Maria Carrillo, the association’s chief science officer, addressed issues of whether Aduhelm works by saying, “One of the questions that you may be asked, or maybe you’re asking yourself is: Is the scientific evidence sufficient to conclude” that Aduhelm and similar monoclonal antibodies “improve health outcomes for Medicare beneficiaries?” The answer, she said, was “yes.”While some patients enthusiastically back the association’s efforts, its stance troubles some longtime supporters of the organization, including Dr. Daniel Gibbs, a retired neurologist in Portland, Ore., with early-stage Alzheimer’s. Dr. Daniel Gibbs, a retired neurologist with early-stage Alzheimer’s, agrees with Medicare’s proposed restrictions on Aduhelm.Amanda Lucier for The New York TimesHe participated in an aducanumab trial, experiencing brain swelling and bleeding that required treatment in an intensive care unit. “I want aducanumab to be successful, and I really think that it might be useful,” he said. However, he added, he considers Medicare’s proposed restrictions appropriate.He called the Alzheimer’s Association campaign “shocking and irresponsible” and said he’ll stop donating to the organization, except for his local chapter. “The vast majority of experts in Alzheimer’s are not on the side of the Alzheimer’s Association,” he said.Several members of the association’s scientific and medical advisory group said they had concluded the drug shouldn’t yet be approved. Still, the association pushed for approval.The F.D.A. itself acknowledged the unclear benefit when it greenlighted Aduhelm under “accelerated approval,” which allows authorization of unproven drugs for serious diseases with few treatments, if the drug affects a biological mechanism in a way considered “reasonably likely to predict clinical benefit.”The agency’s justification was that Aduhelm targets a protein, amyloid, that forms plaques in the brains of Alzheimer’s patients. But many Alzheimer’s experts say that years of data have not shown that reducing amyloid can slow cognitive decline.In the association staff meeting, Dr. Carrillo described experts who criticized Aduhelm’s approval as “naysayers” who “are mainly anti-amyloid researchers, in conflict, in my view.”Several scientists critical of Aduhelm’s approval support the idea that targeting amyloid might help patients; they simply found Aduhelm’s results unconvincing.Mr. Egge, the chief public policy officer, did say at one meeting: “It’s not certain that this first treatment will work, certainly, for everybody, but it could.” He said that it’s common to have “first treatments making marginal differences” but that later drugs often work better. Mr. Johns said the association and its lobbying affiliate, the Alzheimer’s Impact Movement, have spent hundreds of thousands of dollars on the campaign.At the staff meeting, Mr. Johns addressed another issue: “Of course, you’ll hear people claim that we’re doing this because we receive some funding from the pharmaceutical industry or these companies.”He said corporate contributions “are very small, less than 1 percent of our total revenue,” adding, “We would never be affected by any kind of fund-raising.”One attendee asked: “Since the amount of funding we receive from biotech companies is so low, why not refuse to take it and take away the appearance of possible conflicts of interest?”Mr. Johns replied, “We’ve contemplated this many times,” but concluded it would have unintended consequences, like preventing the organization from accepting corporate matching contributions for participants in association fund-raising walks who happened to work at pharmaceutical companies.In the interview, Mr. Johns echoed these explanations. Asked if association officials had communicated with Biogen since Medicare’s proposal, he said, “I think probably some of our folks have had a conversation or more along the way” and that Biogen’s staff “occasionally pass along a piece of information, but I can tell you that we just don’t coordinate with them.”In the recordings, association officials told advocates that their annual meetings with local members of Congress would involve different “asks” than usual: They should request that lawmakers give a floor speech, write to C.M.S., or post on social media to urge Medicare to broadly cover Aduhelm and any other F.D.A.-approved Alzheimer’s treatment.One official, Jennifer Pollack, suggested that advocates should give congressional staff a “leave-behind” that included a sample letter, and social media posts drafted by the association and “sample talking points for a floor speech.”Kate Johnson, another official, told advocates: “If you do not know the answer to a question, that is totally OK.” In that case, “please always revert to our safest phrase,” which, she said, was: “‘I’m not sure, but I can pass that question on to a staffer at the Alzheimer’s Association who can provide some more information.’”She also urged advocates to take photos or screenshots of the congressional meetings to post on social media, tagging the lawmaker to show “we’re not going to give up on the issues that we’re passionate about.”Christopher Masak, director of advocacy, role-played being an Alzheimer’s patient’s son meeting with a lawmaker.“My mom is living with a fatal disease, and the bottom line is, I want more time,” his character said, adding, “Thinking of people like my mom who can’t access this medication, it just, it breaks my heart.”Medicare officials said that limiting coverage to clinical trial participants is especially important because Aduhelm is intended for people with early mild disease, who could potentially be sacrificing years of remaining function and quality of life if a drug’s harms outweigh any benefit.Mr. Johns said he understood the view that “risk could be better tolerated later in the disease” but said that the milder early period is the time many people most want to try to extend. C.M.S. officials also said Aduhelm data isn’t sufficiently representative because most trial participants were white, while Blacks and Latinos have greater Alzheimer’s risk. So, Medicare’s proposal requires that new clinical trials reflect racial and ethnic diversity.Association officials said Medicare’s proposal could have the opposite effect because people in underserved communities might have less access to clinical trial sites.A few issues mentioned by advocacy groups have also been raised by those who don’t oppose limiting coverage for Aduhelm. One is that, as currently worded, Medicare’s decision would apply to all monoclonal antibodies for Alzheimer’s, several of which are in late-stage trials and may soon be considered for F.D.A. approval.“It is essentially denying access to all current and future F.D.A.-approved treatments targeting amyloid in those living with Alzheimer’s disease,” Ms. Pollack said in one recording.The American Academy of Neurology wrote to C.M.S. calling the proposal to cover only patients in clinical trials “prudently designed to investigate the safety and effectiveness,” but asked that it be limited only to Aduhelm. In a statement, a C.M.S. spokeswoman, Beth Lynk, said coverage criteria could be re-evaluated for subsequent monoclonal antibodies. “C.M.S. intends to be nimble and respond to new evidence as it is made available — especially related to the clinical benefit of future therapeutics,” she said.Mr. Johns, who said that he recently attended three meetings with C.M.S. officials, including one with the agency’s administrator, indicated in the interview that the association wouldn’t be satisfied if Medicare’s restrictions applied only to Aduhelm, saying, “We absolutely believe there is sufficient evidence to provide coverage for the first approved treatment.”Advocacy groups’ efforts have gotten some lawmakers’ attention. Recently, a bipartisan group of 40 House members wrote asking C.M.S. to provide broad coverage.Earlier, 78 House Republicans sent a letter criticizing C.M.S.’s proposal, quoting the Alzheimer’s Association and UsAgainstAlzheimer’s. Both advocacy groups were described on Senator Susan Collins’s website as supporting a letter she and another Republican, Senator Shelley Moore Capito, wrote.Some lawmakers, including Democrats, have tweeted a version of the association’s language.But other lawmakers praised Medicare’s proposal, including Representatives Carolyn B. Maloney and Frank Pallone, Democrats who chair committees investigating the F.D.A.’s approval of Aduhelm.Mr. Johns said he didn’t know of any lawmakers who had switched from supporting to opposing Medicare’s proposal. But he said the association’s congressional meetings “have had positive outcomes, even for people who might still have a different opinion. There is at least a different level of understanding.”He declined to provide the number of tweets, letters or other measures of the campaign’s reach, saying: “There are those who are working against access. We are not inclined to share details of our tactical approaches with them. Our activities will be measured by outcomes that grant those with Alzheimer’s disease access to current and future F.D.A.-approved treatments without unnecessary barriers.”
Read more →