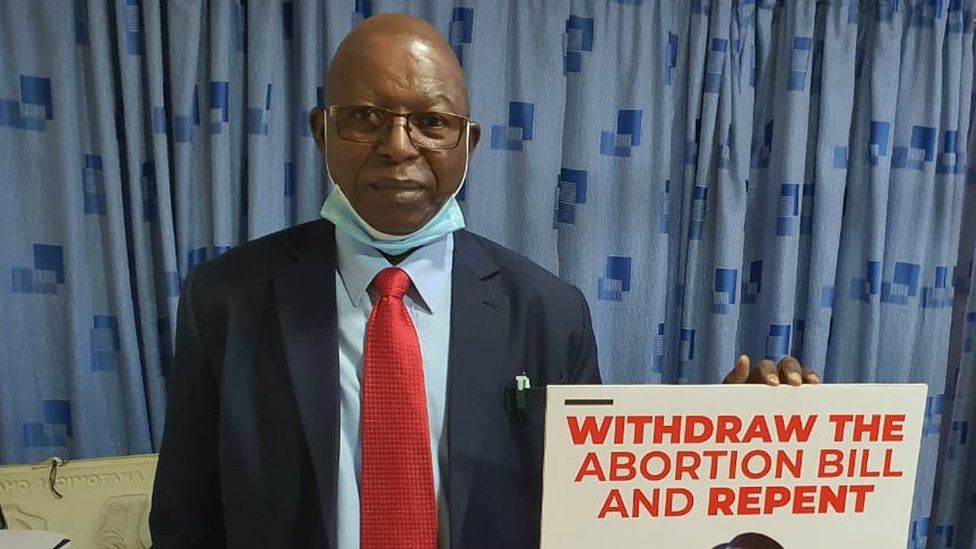
Stephen Karanja: Kenyan anti-vaccine doctor dies from Covid-19
SharecloseShare pageCopy linkAbout sharingimage copyrightCitizenGOA Kenyan doctor who became a vociferous opponent of Covid-19 vaccines has succumbed to the virus, weeks after saying the jabs were “totally unnecessary”. Dr Stephen Karanja, chairman of the Kenya Catholic Doctors Association, advocated steam inhalation and hydroxychloroquine tablets. He clashed with the Catholic church over the safety of Covid jabs.Health authorities and the World Health Organization (WHO) rejected his claims. “[The vaccine] being distributed in Kenya, has been reviewed and found safe not only by the WHO rigorous process but also by several stringent regulatory authorities,” the WHO said in March.Africa Live: Latest updates from across the continentKenyan nurse: ‘I was shunned over coronavirus fears’The women fighting South Africa’s ‘infodemic’The Kenya Conference of Catholic Bishops also distanced itself from Dr Karanja’s view on Covid-19 vaccines, saying the vaccines were “licit and ethically acceptable.” Kenya received just over a million vaccine doses from the global Covax initiative, most of which have been administered. The country has confirmed more than 160,000 cases and 2,707 deaths. In March, the government imposed another lockdown restricting movement in five counties after a surge in new infections.What did Dr Karanja say about Covid vaccines?In a letter dated 3 March Dr Karanja said that “there are drugs that have been repurposed and used effectively to treat Covid-19,” adding that “we also know that vaccination for this disease is totally unnecessary making the motivation suspect.”He went on in different forums to advocate alternative treatments, including steam inhalation and a cocktail of drugs – including hydroxychloroquine and Ivermectin, which have not been approved by the WHO to treat Covid-19.Covid-19 and hydroxychloroquine: What do we know?The South African debate over IvermectinDr Karanja, who was an obstetrician and gynaecologist, died on Thursday a week after he was admitted to hospital suffering from complications caused by a Covid-19 infection.What else has Dr Karanja said?Before falling out with the Catholic church in Kenya about the safety and efficacy of the Covid-19 vaccine, Dr Karanja often allied with the religious leaders to oppose mass vaccination campaigns. In 2019 he led opposition against vaccination of schoolgirls against cervical cancer, saying the jab against Human Papilloma Virus (HPV) was unnecessary because it affected those “whose lifestyle involves irresponsible sexual behaviours”. In 2014, his association opposed the government’s rollout of a tetanus vaccine targeting women, claiming it was a sterilisation campaign, despite local health authorities, the WHO, and the UN children’s agency Unicef saying the vaccine was safe.In both instances the government carried on with its plans, but officials reported that they encountered vaccine hesitancy as a result of the objections raised by Dr Karanja.He was also a prominent anti-abortion campaigner and appeared in court in 2018 as an expert witness in a case in which the government was sued for withdrawing guidelines on abortion. The high court ruled that the government decision was unlawful and illegal. Though shunned by a majority of health professionals in Kenya, the Catholic church recognised his association, but often hastened to add that Dr Karanja did not speak for the Catholic church.”The mandate of the church is to speak on matters of morality and faith. The mandate of the doctors is to speak on their understanding of their scientific practice. We are not at variance,” Father Ferdinand Lugonzo, the Kenya Conference of Catholic Bishops spokesperson, told the BBC.A SIMPLE GUIDE: How do I protect myself?IMPACT: What the virus does to the bodyRECOVERY: How long does it take?
Read more →