Investigation into Covid Origins Sought
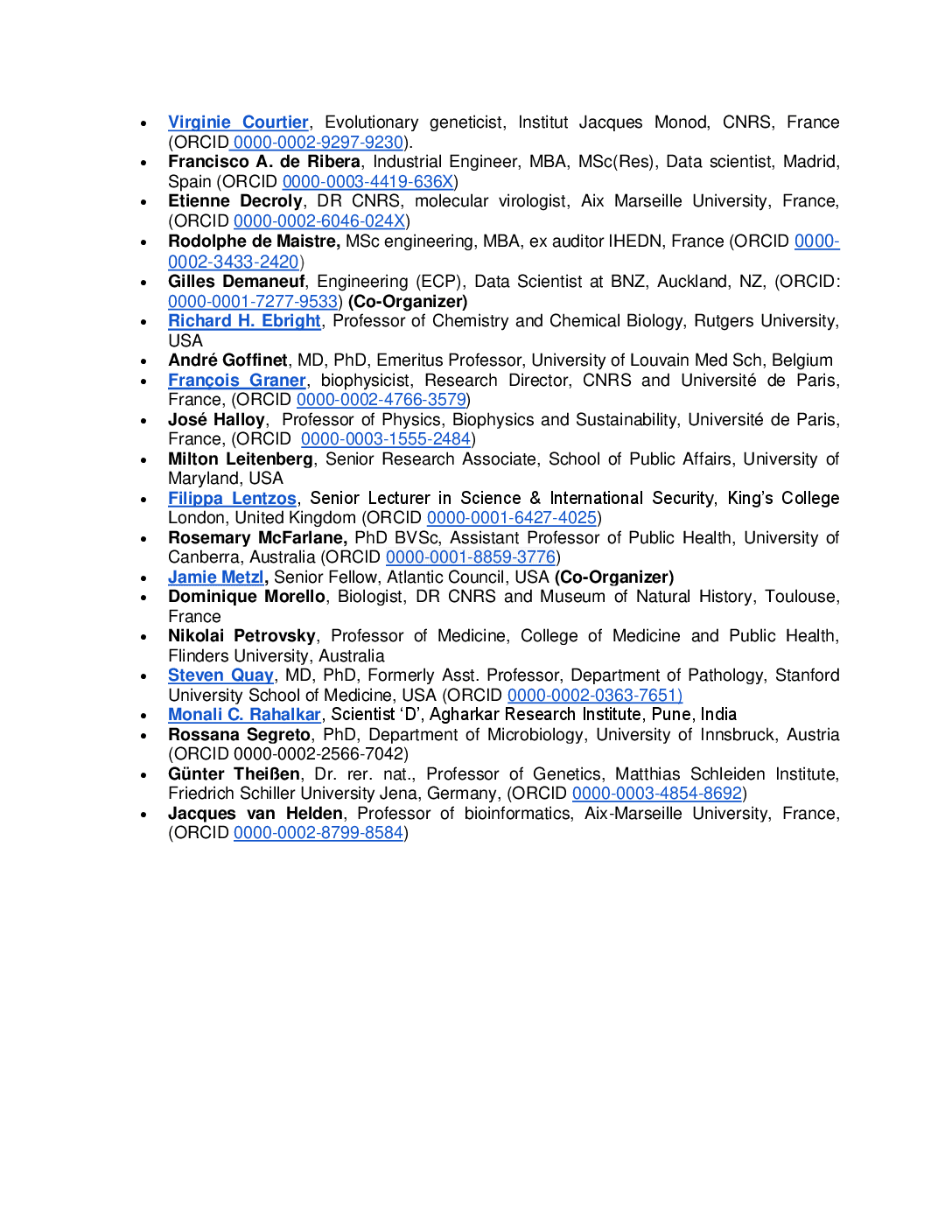
• Virginie Courtier, Evolutionary geneticist, Institut Jacques Monod, CNRS, France (ORCID 0000-0002-9297-9230). • Francisco A. de Ribera, Industrial Engineer, MBA, MSc(Res), Data scientist, Madrid, Spain (ORCID 0000-0003-4419-636X) • Etienne Decroly, DR CNRS, molecular virologist, Aix Marseille University, France, (ORCID 0000-0002-6046-024X) • Rodolphe de Maistre, MSc engineering, MBA, ex auditor IHEDN, France (ORCID 0000- 0002-3433-2420) • Gilles Demaneuf, Engineering (ECP), Data Scientist at BNZ, Auckland, NZ, (ORCID: 0000-0001-7277-9533) (Co-Organizer) • Richard H. Ebright, Professor of Chemistry and Chemical Biology, Rutgers University, USA • André Goffinet, MD, PhD, Emeritus Professor, University of Louvain Med Sch, Belgium • François Graner, biophysicist, Research Director, CNRS and Université de Paris, France, (ORCID 0000-0002-4766-3579) • José Halloy, Professor of Physics, Biophysics and Sustainability, Université de Paris, France, (ORCID 0000-0003-1555-2484) • Milton Leitenberg, Senior Research Associate, School of Public Affairs, University of Maryland, USA • Filippa Lentzos, Senior Lecturer in Science & International Security, King’s College London, United Kingdom (ORCID 0000-0001-6427-4025) • Rosemary McFarlane, PhD BVSc, Assistant Professor of Public Health, University of Canberra, Australia (ORCID 0000-0001-8859-3776) • Jamie Metzl, Senior Fellow, Atlantic Council, USA (Co-Organizer) • Dominique Morello, Biologist, DR CNRS and Museum of Natural History, Toulouse, France • Nikolai Petrovsky, Professor of Medicine, College of Medicine and Public Health, Flinders University, Australia • Steven Quay, MD, PhD, Formerly Asst. Professor, Department of Pathology, Stanford University School of Medicine, USA (ORCID 0000-0002-0363-7651) • Monali C. Rahalkar, Scientist ‘D’, Agharkar Research Institute, Pune, India • Rossana Segreto, PhD, Department of Microbiology, University of Innsbruck, Austria (ORCID 0000-0002-2566-7042) • Günter Theißen, Dr. rer. nat., Professor of Genetics, Matthias Schleiden Institute, Friedrich Schiller University Jena, Germany, (ORCID 0000-0003-4854-8692) • Jacques van Helden, Professor of bioinformatics, Aix-Marseille University, France, (ORCID 0000-0002-8799-8584)
Read more →