Do We Still Need to Keep Wearing Masks Outdoors?
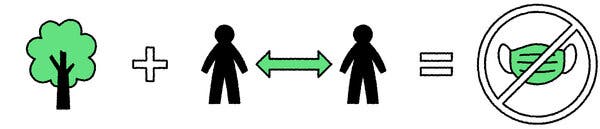
Science shows that the risk of viral transmission outside is very low. The “two-out-of-three rule” can help you decide whether to mask up.As more people get vaccinated and spring weather and sunshine beckon us outdoors, one question may be nagging at you: Do we still need to wear masks outside?More than a year into pandemic life, many people remain confused about the risk of spending time outdoors around other people. A growing body of research shows that transmission of Covid-19 is far less likely outdoors than inside, and the risk will get even lower as more people get vaccinated and cases continue to decline. But many states have yet to lift strict outdoor mask mandates. In Massachusetts, for instance, outdoor masking is required at all times, even when nobody else is around.Recently the online magazine Slate stirred controversy when it suggested an end to outdoor mask rules. The article won support from top public health experts and even The New England Journal of Medicine blog but prompted a fierce backlash from readers, who noted that while the risk of outdoor transmission may be low, it’s not zero.“Shallow and selfish take,” wrote one reader on Twitter. “You have blood on your hands. You should feel ashamed,” posted another.After a year in which many of us have learned to dutifully wear masks and look askance at anyone who does not, it’s understandable that people remain fearful when they cross paths with the unmasked. So how do you make the right decision about when to wear a mask outside?Many virus and public health experts say the guidance hasn’t changed — spending time with others outside during the pandemic has always been safer than indoors. But whether a mask is needed outdoors depends on the circumstances, including local public health rules. Brief encounters with an unmasked person passing you on the sidewalk or a hiking trail are very low risk, said Linsey Marr, a professor of civil and environmental engineering at Virginia Tech. Viral particles quickly disperse in outdoor air, and the risk of inhaling aerosolized virus from a jogger or passers-by are negligible, she said. Even if a person coughs or sneezes outside as you walk by, the odds of you getting a large enough dose of virus to become infected remain low, she said.“I think the guidelines should be based on science and practicality,” said Dr. Marr. “People only have so much bandwidth to think about precautions. I think we should focus on the areas that have highest risk of transmission, and give people a break when the risk is extremely low.”Dr. Marr uses a simple two-out-of-three rule for deciding when to wear a mask. In every situation, she makes sure she’s meeting two out of three conditions: outdoors, distanced and masked. “If you’re outdoors, you either need to be distanced or masked,” she said. “If you’re not outdoors, you need to be distanced and masked. This is how I’ve been living for the past year. It all comes down to my two-out-of-three rule.”Use the 2-out-of-3 RuleTo lower risk for Covid-19, make sure your activity meets two out of the following three conditions: outdoors, distanced and masked.Outdoors + Distanced = No Mask NeededOutdoors + No Distance = Mask NeededNot Outdoors + Distanced = Mask NeededWhen masks are needed outdoorsIf you stop to have an extended conversation with someone who isn’t vaccinated, masks are recommended. Even outdoors, your risk of breathing someone else’s air increases the longer and closer you stand to them. One of the few documented cases of outdoor transmission happened in China early in the pandemic, when a 27-year-old man stopped to chat outside with a friend who had just returned from Wuhan, where the virus originated. Seven days later, he had his first symptoms of Covid-19.And masks are still advised if you find yourself in an outdoor crowd. Standing shoulder to shoulder with strangers during an outdoor concert or a protest could increase risk, particularly for the unvaccinated.Recently while hiking without a mask, Dr. Marr said she still made an effort to keep her distance from large groups when the trail got crowded.“If I was passing by a solo hiker it didn’t concern me,” said Dr. Marr. “But if I passed by a group of 10 hikers in a row, I stepped further off the path. The risk is still low, but at some point there could be a large enough pack of people that the risk could become appreciable.”When outdoor risk is lowestWalking your dog, riding a bike, hiking on a trail or picnicking with members of your household or vaccinated friends are all activities where the risk for virus exposure is negligible. In these kinds of situations, you can keep a mask on hand in your pocket, in case you find yourself in a crowd or need to go indoors..css-1xzcza9{list-style-type:disc;padding-inline-start:1em;}.css-rqynmc{font-family:nyt-franklin,helvetica,arial,sans-serif;font-size:0.9375rem;line-height:1.25rem;color:#333;margin-bottom:0.78125rem;}@media (min-width:740px){.css-rqynmc{font-size:1.0625rem;line-height:1.5rem;margin-bottom:0.9375rem;}}.css-rqynmc strong{font-weight:600;}.css-rqynmc em{font-style:italic;}.css-yoay6m{margin:0 auto 5px;font-family:nyt-franklin,helvetica,arial,sans-serif;font-weight:700;font-size:1.125rem;line-height:1.3125rem;color:#121212;}@media (min-width:740px){.css-yoay6m{font-size:1.25rem;line-height:1.4375rem;}}.css-1dg6kl4{margin-top:5px;margin-bottom:15px;}.css-16ed7iq{width:100%;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;-webkit-box-pack:center;-webkit-justify-content:center;-ms-flex-pack:center;justify-content:center;padding:10px 0;background-color:white;}.css-pmm6ed{display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}.css-pmm6ed > :not(:first-child){margin-left:5px;}.css-5gimkt{font-family:nyt-franklin,helvetica,arial,sans-serif;font-size:0.8125rem;font-weight:700;-webkit-letter-spacing:0.03em;-moz-letter-spacing:0.03em;-ms-letter-spacing:0.03em;letter-spacing:0.03em;text-transform:uppercase;color:#333;}.css-5gimkt:after{content:’Collapse’;}.css-rdoyk0{-webkit-transition:all 0.5s ease;transition:all 0.5s ease;-webkit-transform:rotate(180deg);-ms-transform:rotate(180deg);transform:rotate(180deg);}.css-eb027h{max-height:5000px;-webkit-transition:max-height 0.5s ease;transition:max-height 0.5s ease;}.css-6mllg9{-webkit-transition:all 0.5s ease;transition:all 0.5s ease;position:relative;opacity:0;}.css-6mllg9:before{content:”;background-image:linear-gradient(180deg,transparent,#ffffff);background-image:-webkit-linear-gradient(270deg,rgba(255,255,255,0),#ffffff);height:80px;width:100%;position:absolute;bottom:0px;pointer-events:none;}#masthead-bar-one{display:none;}#masthead-bar-one{display:none;}.css-1pd7fgo{background-color:white;border:1px solid #e2e2e2;width:calc(100% – 40px);max-width:600px;margin:1.5rem auto 1.9rem;padding:15px;box-sizing:border-box;}@media (min-width:740px){.css-1pd7fgo{padding:20px;width:100%;}}.css-1pd7fgo:focus{outline:1px solid #e2e2e2;}#NYT_BELOW_MAIN_CONTENT_REGION .css-1pd7fgo{border:none;padding:20px 0 0;border-top:1px solid #121212;}.css-1pd7fgo[data-truncated] .css-rdoyk0{-webkit-transform:rotate(0deg);-ms-transform:rotate(0deg);transform:rotate(0deg);}.css-1pd7fgo[data-truncated] .css-eb027h{max-height:300px;overflow:hidden;-webkit-transition:none;transition:none;}.css-1pd7fgo[data-truncated] .css-5gimkt:after{content:’See more’;}.css-1pd7fgo[data-truncated] .css-6mllg9{opacity:1;}.css-1rh1sk1{margin:0 auto;overflow:hidden;}.css-1rh1sk1 strong{font-weight:700;}.css-1rh1sk1 em{font-style:italic;}.css-1rh1sk1 a{color:#326891;-webkit-text-decoration:underline;text-decoration:underline;text-underline-offset:1px;-webkit-text-decoration-thickness:1px;text-decoration-thickness:1px;-webkit-text-decoration-color:#ccd9e3;text-decoration-color:#ccd9e3;}.css-1rh1sk1 a:visited{color:#333;-webkit-text-decoration-color:#ccc;text-decoration-color:#ccc;}.css-1rh1sk1 a:hover{-webkit-text-decoration:none;text-decoration:none;}“I think it’s a bit too much to ask people to put the mask on when they go out for a walk or jogging or cycling,” said Dr. Muge Cevik, a clinical lecturer of infectious disease and medical virology at the University of St. Andrews School of Medicine in Scotland, where outdoor masking has never been required. “We’re in a different stage of the pandemic. I think outdoor masks should not have been mandated at all. It’s not where the infection and transmission occurs.”“Let me go for my run, maskless. Mask in pocket,” tweeted Dr. Nahid Bhadelia, an infectious diseases physician and the medical director of the special pathogens unit at Boston Medical Center. “Given how conservative I have been on my opinions all year, this should tell you how low risk is, in general, for outdoors transmission for contact over short periods — and lower still after vaccination. Keep the masks on you for when you are stationary in a crowd and headed indoors.”To understand just how low the risk of outdoor transmission is, researchers in Italy used mathematical models to calculate the amount of time it would take for a person to become infected outdoors in Milan. They imagined a grim scenario in which 10 percent of the population was infected with Covid-19. Their calculations showed that if a person avoided crowds, it would take, on average, 31.5 days of continuous outdoor exposure to inhale a dose of virus sufficient to transmit infection.“The results are that this risk is negligible in outdoor air if crowds and direct contact among people are avoided,” said Daniele Contini, senior author of the study and an aerosol scientist at the Institute of Atmospheric Sciences and Climate in Lecce, Italy.Even as more-infectious virus variants circulate, the physics of viral transmission outdoors haven’t changed, and the risk of getting infected outdoors is still low, say virus experts. Pay attention to the rates of infection in your community. If case counts are surging, your risk of encountering an infected person goes up.When outdoor fun moves indoorsDr. Cevik notes that debates about outdoor masking and articles showing photos of crowded beaches during the pandemic have left people with the wrong impression that parks and beaches are unsafe, and distracted from the much higher risks of indoor transmission. Often it’s the indoor activities associated with outdoor fun — like traveling unmasked in a subway or car to go hiking, or dropping into a pub after spending time at the beach — that pose the highest risk. “People hold barbecues outdoors, but then they spend time indoors chatting in the kitchen,” said Dr. Cevik.As more people get vaccinated, decisions about going maskless outdoors will get easier. While no vaccine offers 100 percent protection, the rate of breakthrough infections so far has been exceedingly low. The U.S. Centers for Disease Control and Prevention recently reported just 5,800 cases of breakthrough infections among 75 million vaccinated people. And the C.D.C. has said vaccinated friends and family members can safely spend time together, without masks.But it’s OK to keep wearing your mask outdoors if you prefer it. After a year of taking pandemic precautions, it may be hard for people to adjust to less restrictive behaviors. Sarit A. Golub, a psychology professor at Hunter College of the City University of New York, said it’s important for both the media and public health officials to communicate the reasons people can modify some behaviors, like outdoor masking.“In the coming months, ‘normal life’ will begin to become safer, but I worry that some people won’t be willing or able to relax pandemic restrictions in ways that makes sense,” Dr. Golub said. “I worry that folks have internalized the fear messaging without understanding the reasons behind specific behavioral recommendations, and therefore, the reasons that they can be modified as circumstances change.”Gregg Gonsalves, assistant professor of epidemiology at the Yale School of Public Health, said he recently was with a group of parents, including many vaccinated physicians, who met in a New Haven park to celebrate a child’s first birthday. “We’re all just standing around, everybody was masked, and then we started asking, ‘When’s the time we can be outside and take off our masks?’” Dr. Gonsalves said. “If people are vaccinated and you’re outdoors, masks are probably superfluous at this point.”But Dr. Gonsalves said he understands why some people may be reluctant to give up their masks outdoors. “Some of this is Covid hangover,” he said. “We’ve been so traumatized by all of this. I think we need to have a little bit of compassion for the people having trouble letting go.”Illustrations by Eden Weingart
Read more →