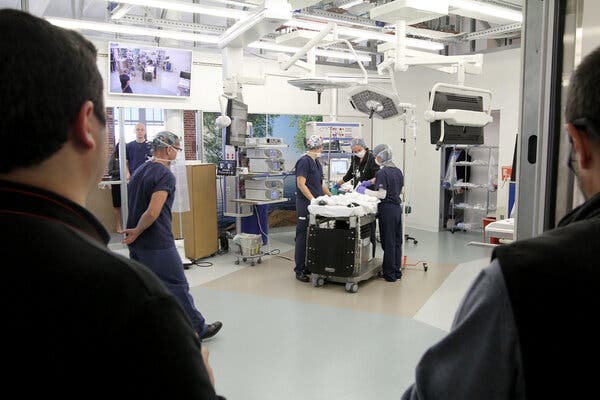
Hospitals are bringing together surgeons, anesthesiologists and nurses with architects, engineers and administrative staff to rethink the modern operating room.This article is part of our new series on the Future of Health Care, which examines changes in the medical field.If you ask Dr. Scott T. Reeves, operating rooms resemble an airplane cockpit. There is sophisticated equipment, tight spaces, blinking lights and a cacophony of sound.On top of that, “they’re often cluttered, people can trip, surgeons and nurses can stick themselves with needles, and side infections from dust and other contaminations are a growing problem,” said Dr. Reeves, chair of the department of anesthesia and perioperative medicine at the Medical University of South Carolina.When he became involved with the design of the operating rooms at the R. Keith Summey Medical Pavilion, part of the children’s hospital of the university, Dr. Reeves focused on how to make surgical suites more accommodating for technology — including imaging machines and robots — as well as staff and patients.Dr. Reeves’s actions are part of an increasing recognition that hospitals are “human centered,” said Anjali Joseph, the director of the Center for Health Facilities Design and Testing at Clemson University, who worked on the design for the ambulatory center that opened in 2019. “We cannot think of patient safety without thinking about the health of everyone in the room. They are interlinked.”Their goal: to rethink the layout as well as plan for the future, and the South Carolina team is not alone. The problem of squeezing people and a variety of machines — not to mention robots — into surgical suites designed decades ago is forcing a change.A full-scale simulated pediatric operating room at the Medical University of South Carolina allowed staff members to evaluate what would work best.Sarah Pack/MUSCFrom increasing in size to reorienting the layout, hospitals — especially those that are part of large university medical centers — are bringing together surgeons, anesthesiologists and nurses with architects, engineers and administrative staff to rethink the modern operating room. But even older community hospitals, with more limited budgets, are getting creative, since surgeries are an all-important source of revenue.While new construction is more straightforward than retrofitting an older building, not every hospital has the financing or the space to begin anew. Building a new operating room alone can cost from $1 million to $3 million per surgical suite, Dr. Reeves said. The cost of a new hospital can exceed $1 billion.Configuring new surgical suites in existing buildings requires creativity, said Joan Saba, a health care architect and partner with NBBJ, an architecture and design firm.For example, older operating rooms may have ceiling heights as low as 10 feet, while 12-16 feet is now considered optimum, to house electronics, cables and ductwork, she said. Some have captured space from the floor above to gain the extra height. Where that is not an option, some hospitals have repurposed adjoining rooms to house electronics and other infrastructure.New equipment and new surgical techniques are largely driving the redesigns. Those designing operating rooms even 20 years ago could not have foreseen the explosion in technology, which often requires more space.“Imaging management” is the biggest challenge that operating rooms have, said Mary Hawn, the chair of the department of surgery at Stanford University, which opened a new hospital in November 2019 (Stanford’s new children’s hospital opened in 2017). “Twenty years ago we would operate on exactly what we were looking at, possibly magnifying it with loupes,” the specialized glasses that augment a surgeon’s vision. Now, monitors provide high definition to guide the surgeon.In addition, for very complicated surgeries, hospitals hope to have equipment like CT scans and other imaging machines in the operating room. This not only saves time but lessens the risk of infection.“Patients need not be closed up, taken out for imaging, see that you missed something and then bring them back to the operating room and open them up again,” Ms. Saba said.Of all the imaging equipment, the only one generally unsuitable for the operating room is that needed for magnetic resonance imaging — commonly known as an M.R.I. — because of its size. As a result, Ms. Saba said, some hospitals essentially are stationing them adjacent to an operating room in case an M.R.I. is needed. A separate space has an added efficiency benefit, because the equipment can be used for nonsurgical patients as well.Ceilings are not overlooked. Freeing up valuable floor space, monitors are often affixed to ceiling-mounted booms, which can have several arms and may also serve as a conduit for gases needed for anesthesia. Ultraviolet cleaning systems, which eliminate bacteria and viruses, can be anchored in the ceilings, to assist with disinfection. And the space above the ceiling is often larger to house a range of cables and other electronic equipment, in addition to ductwork with sophisticated air filtration systems.Access to the space above the ceiling, as well as behind the walls, has become important, so that any technical problems can be investigated and remedied within hours, rather than shutting a room down for lengthy repairs. Some hospitals, for example, are now considering stainless steel prefabricated wall systems for their surgical suites because they are both easier to clean and easier to take out if the electronics hidden behind break, Ms. Saba said.Other important factors are lighting and noise. When it comes to increasingly common laparoscopic surgery, monitors that guide surgeons are lit but overhead lights may be turned off to reduce glare, Dr. Hawn said.That “can be somewhat dangerous because it can be quite dark and people run into things or trip over things,” she added. “We now have green lighting, which allows us to be able to see a sharp image on the monitors without the glare that you get from the white light.”Noise is distracting at best, but with physical repercussions, like hypertension, especially for staff exposed for long periods. High decibel levels are “associated with increased difficulty in communication, which is the largest source of preventable errors in the hospital environment,” John Medina, an affiliate associate professor at the University of Washington department of bioengineering, said in an email.At the Loma Linda University Medical Center in California, which is expected to open a new hospital on its campus this year, the operating room walls are built to mitigate outside noise as well as vibrations, and air duct silencers are being used as well, said Allison Ong, the head of campus transformation.A renovated operating room at the R. Keith Summey Medical Pavilion gives staff the option to move equipment, lights and monitors around the operating table during surgeries.Sarah Pack/MUSCHospital construction — whether for new buildings or even renovated pre-existing spaces, takes years, from inception to opening and can cost hundreds of millions of dollars. Before the spaces are put into use, all the staff — from the surgeons to the orderlies — need to practice in the new configuration. Dress rehearsals are common, in spaces like warehouses or even parking lots that are mocked up with cardboard walls to resemble the finished surgical suite.A run-through can be elaborate, bringing together surgeons, anesthesiologists and nurses. Several days of full hospital rehearsals, for example, are in the works at the Loma Linda center. The planning for the 500 or more people who will attend each day has itself taken months, Ms. Ong said.Evaluating the finished space before the first patient arrives can also help the medical staff make important choices. The Medical University of South Carolina, was considering a specialized piece of imaging equipment for its children’s hospital that would have permitted a fluoroscopy during surgery, Dr. Reeves said. But the machine had a big footprint, so a group taped it out on the floor.“What we realized by doing that was that it greatly decreased the functionality of the room for routine cardiac surgical patients,” he said. “It was great for the 10-15 patients a year we would potentially need it for, but it substantially became a burden for everyone else.” The hospital decided against installing the equipment in the operating room itself.Over all, perhaps the biggest question in these renovations is how to “future proof” the operating rooms, in addition to the overall hospital. It is a particularly challenging exercise with technology changing so rapidly.At Loma Linda, Ms. Ong said, “We had to decide very early on what the future of health care was going to look like. How many I.C.U. beds, how many medical surgical beds and how many O.R’s. You make your best guess.”Part of that is adopting a more modular approach, to allow flexibility for new equipment. As Dr. Reeves said: “The takeaway from Covid is how rigid many operating rooms are. I think you’ll see a lot of architecture firms be more nimble in their designs. And while that comes with an increased cost, it’s a question of either pay me now or pay me later.”
Read more →