How ‘laughing gas’ became a deadly – but legal – American addiction
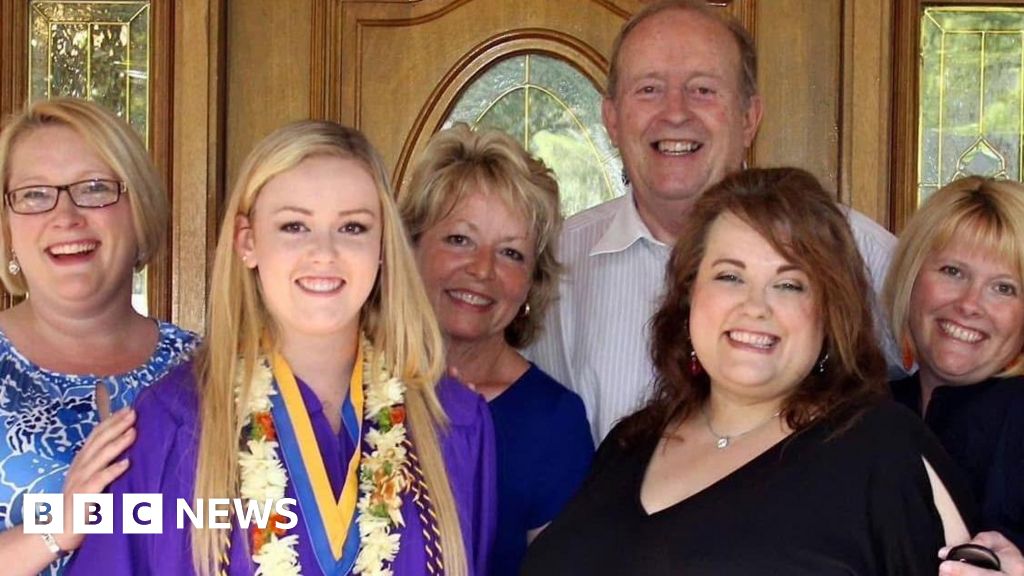
Nitrous oxide – known colloquially as “laughing gas” – has many uses, from a painkiller during dental procedures to a whipping agent for canned whipped cream.While its euphoric side effects have long been known, the rise of vaping has helped create a perfect delivery vehicle for the gas – and a perfect recipe for an addiction, experts warn.Meg Caldwell’s death wasn’t inevitable.The horseback rider from Florida had started using nitrous oxide recreationally in university eight years ago. But like many young people, she started to use more heavily during the pandemic.The youngest of four sisters, she was was “the light of our lives,” her sister Kathleen Dial told the BBC.But Ms Caldwell’s use continued to escalate, to the point that her addiction “started running her life”.She temporarily lost use of her legs after an overdose, which also rendered her incontinent. Still, she continued to use, buying it in local smoke shops, inhaling it in the car park and then heading straight back into the shop to buy more. She sometimes spent hundreds of dollars a day.She died last November, in one of those car parks just outside a vape shop.”She didn’t think that it would hurt her because she was buying it in the smoke shop, so she thought she was using this substance legally,” Ms Dial said.The progression of Ms Caldwell’s addiction – from youthful misuse to life-threatening compulsion – has become increasingly common. The Annual Report of America’s Poison Centers found there was a 58 % increase in reports of intentional exposure to nitrous oxide in the US between 2023-2024.In a worst-case scenario, inhalation of nitrous oxide can lead to hypoxia, where the brain does not get enough oxygen. This can result in death. Regular inhalation can also lead to a Vitamin B12 deficiency which can cause nerve damage, degradation of the spinal column and even paralysis. The number of deaths attributed to nitrous oxide poisonings rose by more than 110% between 2019 and 2023, according to the Centers for Disease Control and Prevention.Possession of nitrous oxide was criminalised in the UK in 2023 after misuse among young people increased during the pandemic. But while many states have also outlawed the recreational use of the product in the US, it is still legal to sell as a culinary product. Only Louisiana has totally banned the retail sale of the gas.Galaxy Gas, a major manufacturer, even offers recipes for dishes, including Chicken Satay with Peanut Chili Foam and Watermelon Gazpacho on their website. With flavours like Blue Raspberry or Strawberries and Cream, experts warn this loophole – as well as major changes in packaging and retail – has contributed to the rise in misuse.Until recently users would take single-use plain metal canisters weighing around 8g and inhale the gas using a balloon. But when usage spiked during the pandemic, nitrous oxide manufacturers began selling much larger canisters online – as large as 2kg – and, eventually, in shops selling electronic vapes and other smoking paraphernalia.Companies also began to package the gas in bright colourful canisters with designs featuring characters from computer games and television series.Pat Aussem, of the Partnership to End Addiction, believes these developments are behind increased misuse:”Even being called Galaxy Gas or Miami Magic is marketing,” she said. “If you have large canisters, then it means that more people can try it and use it and that can lead to a lot of peer pressure.”The BBC reached out for comment to both Galaxy Gas and Miami Magic but did not receive a response. Amazon, where the gas is sold online, has said they are aware of customers misusing nitrous oxide and that they are working to implement further safety measures. In a response to reporting from CBS News, the BBC’s news partner in the US, Galaxy Gas maintained that the gas was intended for culinary use and that they include a message on their sites warning against misuse.Concern about nitrous oxide misuse increased last year, after several videos of people using the product went viral online.On social media, videos of young people getting high on gas became a trend. A video uploaded in July 2024 by an Atlanta-based fast-food restaurant featured a young man inhaling Strawberries and Cream flavoured nitrous oxide saying “My name’s Lil T, man”, his voice made deeper by the gas. To date the clip has been viewed about 40 million times and spawned thousands of copies.Misuse also featured heavily in rap music videos and Twitch streaming. Guests tried it on the Joe Rogan Show and rappers including Ye (formerly Kanye West) spoke about abusing the substance publicly. Ye has since sued his dentist for “recklessly” supplying Ye with “dangerous amounts of nitrous oxide”.In response to the trend, TikTok blocked searches for “galaxy gas,” and redirected users to a message offering resources about substance use and addiction. Rapper SZA also alerted her social media followers about its harms and slammed it for “being MASS marketed to black children”.In March, the Food and Drug Administration (FDA) issued an official alert warning against inhaling the gas after it “observed an increase in reports of adverse events after inhalation of nitrous oxide products”. The FDA told the BBC that it “continues to actively track adverse events related to nitrous oxide misuse and will take appropriate actions to protect the public health”.But for some, these warnings came too late.In 2023, the family of a 25-year-old woman, Marissa Politte successfully sued Nitrous Distributor United Brands for $745m in damages after the radiology technician was killed by a driver high on nitrous oxide. The jury found the company responsible for selling the product in the knowledge that it would be misused.”Marissa Politte’s death shouldn’t have happened in the first place, but my God, it should be the last,” Johnny Simon, the Politte family’s lawyer, said at the time. In the years since there have been several fatal traffic accidents involving the gas both in the US and the UK.Meanwhile, Ms Caldwell’s family have launched a class action lawsuit against manufacturers and distributors of nitrous oxide, hoping to remove the product from retail sales across the US for good.”The people who administer nitrous oxide in a dentist office now have to go through hours and hours of training, she said. “It just is crazy to me that the drug can be purchased in a smoke shop to anyone who goes in.””Unfortunately, it’s become very obvious that the manufacturers and the owners of the smoke shops are not going to do the moral thing and take this off the shelves themselves,” Ms Dial said.
Read more →