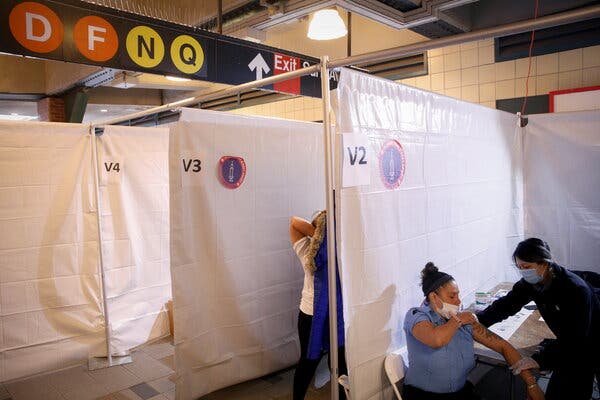
Start with a web search. Consider a third-party tool. Expect frustration.This year, some Americans can do something that was previously impossible: look up the price of care before going to the hospital.A new federal rule requires hospitals to post the prices they negotiate with private insurers.The data is a rich source of new information. We used it to show that some insurers are paying twice or three times as much as their competitors for basic services — and that paying cash rather than using your coverage can often lead to a lower price.But most hospitals have not yet posted the required data. Even when they have, finding it can take time and legwork. Also, you may need to be a computer programmer to open it.“Get some coffee and hydrate, because it’s going to be a while,” said Touré McCluskey, a co-founder of the health start-up Redu Health, which has collected some of the data files. “There is information out there, but it’s not consumer-friendly.”To help those who want to try, we interviewed several researchers who have spent months collecting the data. They recommended several simple strategies.What you’ll need to know to startBefore you start looking for prices, you’ll want to know what kind of health insurance you have — both the name of your insurer and also details like whether you picked an H.M.O. plan during open enrollment or went with a P.P.O. option.Insurers often have a half-dozen rates within the same hospital. Some are specific to which plan you picked and to whether you bought the insurance through the Obamacare marketplace or a specific employer. Others have to do with what network you opted into when you signed up for coverage.Knowing the type of insurance you have will help you make the most sense of which prices in the data apply to you.Then do a web searchFor most hospitals, the data is posted on a page labeled “price transparency.” Many researchers say they begin looking for price files through a search on Google for that phrase and the hospital’s name.“That search should lead you to a top result that has something to do with price estimates billing, or patient information,” said Morgan Henderson, a health economist at the University of Maryland-Baltimore County who worked with The Upshot to collect the price files used in our recent articles. “Sometimes what you want is way at the bottom of that page, or you have to follow a few links.”The page should look something like this one from MedStar Hospital Center, the largest hospital in Washington, D.C.The hospital’s price transparency site will probably have multiple sections and links, and the labeling of the price files isn’t always clear. You’ll want to look for something like a “comprehensive machine-readable file” or “negotiated price list.”It’s also worth opening up files that are described as containing “standard charges” or a “chargemaster.” Here’s how those look at Indiana University Health:When you open the files, you see it actually has the hospital’s negotiated rates and cash prices, too.Here’s what you’re looking forThe government has not created a standard format for hospitals to report their price data, and each hospital seems to take a slightly different approach.Some post their data in Excel or CSV files, which you can open using free software like Google Sheets. But some use JSON files, a data format typically used by computer programmers and professional data scientists that ordinary people might struggle to open.“I have training in health economics and policy, and I’m working on a machine with a lot of memory space,” said Morgane Mouslim, also a health economist at the University of Maryland-Baltimore County, who helped The Upshot collect and standardize data files. “If a file isn’t in Excel, you might need additional software.”A typical data set lists prices by procedure for each insurer, like this one from the Hospital of the University of Pennsylvania:The five-digit figures to the very left of this spreadsheet are CPT codes, which hospitals use to describe each service they offer. Most files also have short descriptions for each code, but they can be confusing. Code U0003, for example, is translated as “PR COV 19 AMP PRB HIGH THRUPUT” — a jargony way of describing a coronavirus test.To look up the cost of a specific service you expect to get at a hospital, you most likely have to call the facility and ask what CPT codes it will bill for your visit.You may also see other numerical codes, sometimes labeled procedure codes or revenue codes, like in the file below from Baptist Medical Center in Little Rock, Ark. You probably don’t need to pay much attention to those and should focus on the CPT codes. (If the CPT codes are not labeled, you can generally recognize them as the ones that are five digits.)Usually, you should see dollar figures representing real prices. But you could run across files where the price is listed as “variable,” meaning it could differ for two patients with the same insurance who received the same care under different circumstances.Molly Smith, vice president for public policy at the American Hospital Association, gave the example of a patient who comes to the hospital for a flu vaccine versus one who happens to get one while there for surgery.“In the contract we generally negotiate the price of the primary service, but if it’s a secondary service, maybe 15 percent is taken off,” she said. “It’s not possible to reflect that in these files.”The files should also include two other prices: the “charge” or “gross price,” which is the sticker price for a given service that hospitals often use as a baseline for negotiating discounts. There should also be the “cash” price, which is what the hospital bills patients who don’t use insurance. Whether this price is available to patients with insurance varies from hospital to hospital. Some low-income patients may qualify for even steeper discounts based on how little they earn.Once you find the data point you’re looking for, there may be additional work to understand it. Most hospitals list the prices as dollar figures, but some display the data as a percent of the gross charge — meaning patients will need to do math to understand their costs.What if I can’t find anything?Most hospitals have not posted the required data, so that may happen a lot.For example, on N.Y.U. Langone’s price transparency website, you can find only standard charges and a patient estimator tool, which uses information about your insurance plan to generate a custom estimate of how much you’ll pay for a certain procedure.Those tools provide limited information. The standard charges can tell you the maximum you could pay for a given service, and the patient estimator shows the out-of-pocket costs associated with simple services like mammograms and blood tests. When a Times reporter tried to use N.Y.U.’s site in late July, however, it generated error messages for all services explored.A representative for N.Y.U. Langone declined to comment on why the hospital had not posted its full data.With compliance rates still low, the federal government is promising to increase enforcement. It has sent nearly 170 warning letters to noncompliant hospitals, and plans to increase the penalties for noncompliance from $109,500 annually to as much as $2 million.If you believe a hospital has not posted the required information, you can file a complaint with the federal government notifying it of the issue.Soon, third-party sites might helpSome health care experts say the large data files will become more useful after third-party data companies clean and organize the information, so that patients can search across multiple hospitals and health care services.One data transparency company, Turquoise Health, has already created a free price lookup tool. Others are expected soon.See something surprising? Tell us about it.The Times has looked into data sets from 60 hospitals so far. But many more are out there.If you notice something surprising in a hospital price file — exceptionally high prices, for example, or large variations in what a service costs — we’d love to hear about it. You can email us with what you’ve found.
Read more →