The Powerful Companies Driving Local Drugstores Out of Business
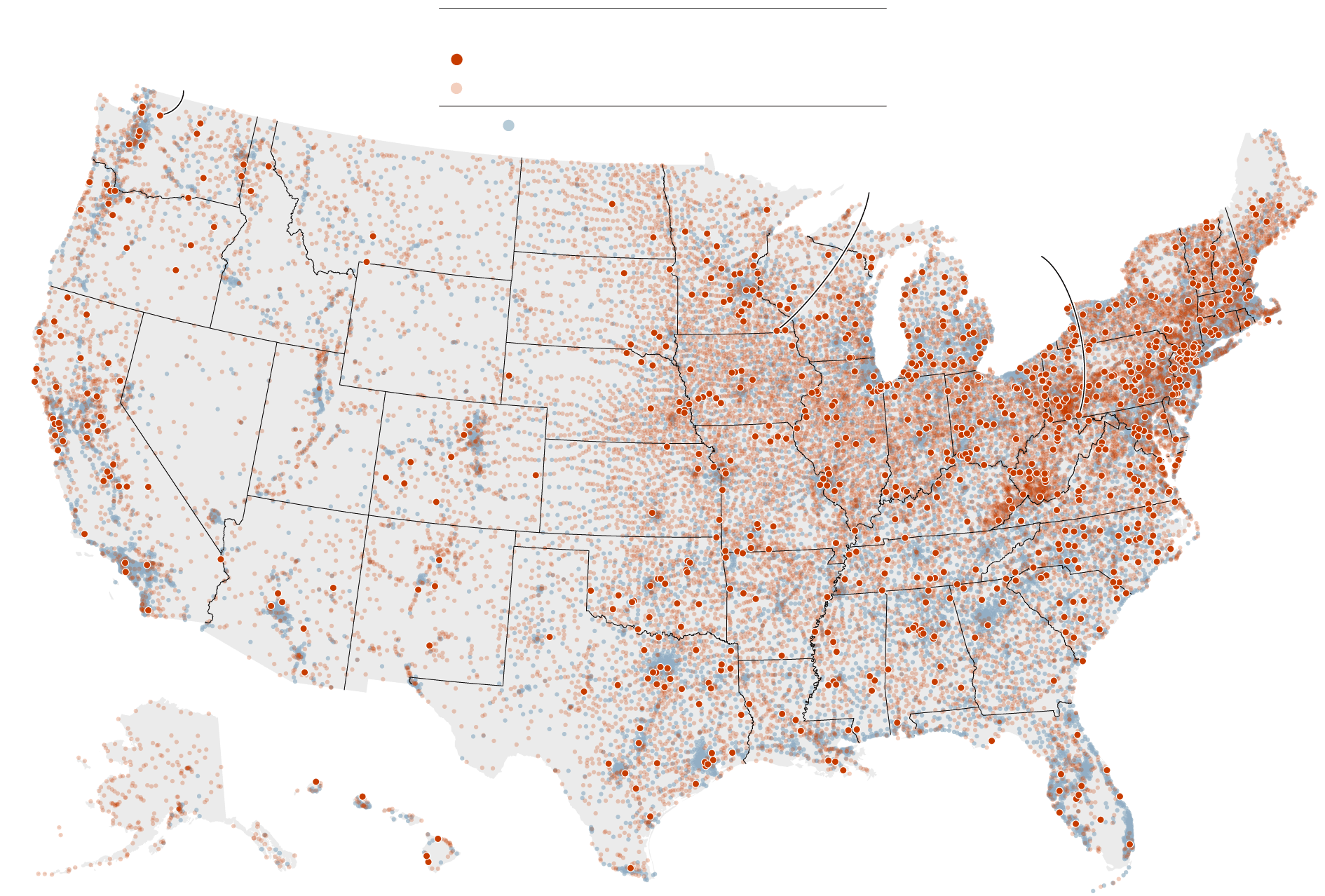
The small-town drugstore closed for the last time on a clear and chilly afternoon in February. Jon Jacobs, who owned Yough Valley Pharmacy, hugged his employees goodbye. He cleared the shelves and packed pill bottles into plastic bins.Mr. Jacobs, a 70-year-old pharmacist, had spent more than half his life building his drugstore into a bedrock of Confluence, Pa., a rural community of roughly 1,000 people. Now the town was losing its only health care provider.Obscure but powerful health care middlemen — companies known as pharmacy benefit managers, or P.B.M.s — had destroyed his business.This has been happening all over the country, a New York Times investigation found. P.B.M.s, which employers and government programs hire to oversee prescription drug benefits, have been systematically underpaying small pharmacies, helping to drive hundreds out of business.The pattern is benefiting the largest P.B.M.s, whose parent companies run their own competing pharmacies. When local drugstores fold, the benefit managers often scoop up their customers, according to dozens of patients and pharmacists.Jon Jacobs packed up medicine on the day he closed his pharmacy in February.Jeff Swensen for The New York TimesMr. Jacobs hugged an employee.Jeff Swensen for The New York TimesNewly Created DesertsNearly 800 ZIP codes that had at least one pharmacy in 2015 now have none.
Read more →