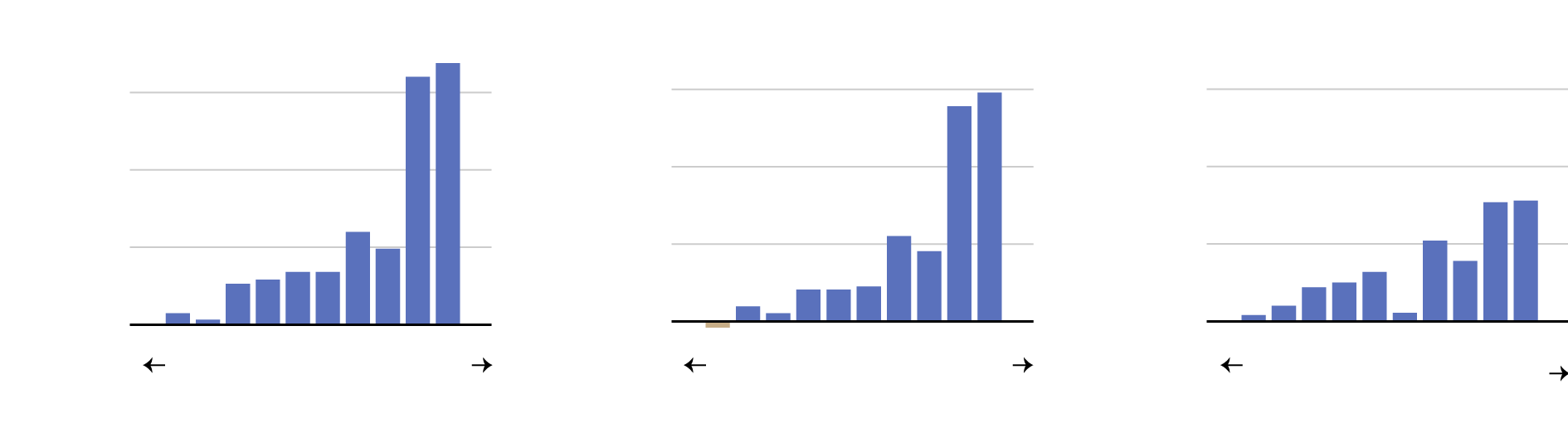
A new study finds that private equity firms own more than half of all specialists in certain U.S. markets.In recent years, private equity firms have been gobbling up physician practices to form powerful medical groups across the country, according to a new report released Monday.In more than a quarter of local markets — in places like Tucson, Ariz.; Columbus, Ohio; and Providence, R.I. — a single private equity firm owned more than 30 percent of practices in a given specialty in 2021. In 13 percent of the markets, the firms owned groups employing more than half the local specialists.The medical groups were associated with higher prices in their respective markets, particularly when they controlled a dominant share, according to a paper by researchers at the Petris Center at the University of California, Berkeley, and the Washington Center for Equitable Growth, a progressive think tank in Washington, D.C. When a firm controlled more than 30 percent of the market, the cost of care in three specialties — gastroenterology, dermatology, and obstetrics and gynecology — increased by double digits.When Private Equity Takes OverResearchers found that when a firm controlled more than 30 percent of the market, the prices paid by private insurers for gastroenterology and other specialties increased sharply.
.dw-chart-subhed {
line-height: 1;
margin-bottom: 6px;
font-family: nyt-franklin;
color: #121212;
font-size: 15px;
font-weight: 700;
}
Average price of gastroenterology visit
Source: Nicholas C. Petris Center on Health Care Markets and Consumer Welfare, University of
California, Berkeley; Washington Center for Equitable GrowthBy The New York TimesThe paper, published by the American Antitrust Institute, documented substantial private equity purchases across multiple medical specialties over the last decade. Urology, ophthalmology, cardiology, oncology, radiology and orthopedics have also been major targets for such deals.“It’s shocking when you look at it,” said Laura Alexander, director of markets and competition policy for the Washington Center, who said private equity firms dominated only a handful of markets a decade ago. By looking at individual markets, the researchers were able to document the local impact. “National rates mask this much more acute problem in local markets,” she said.The higher prices paid by private insurers contribute to high insurance premiums, and may increase out-of-pocket costs for patients.Private equity firms, which pool funds from institutional investors and individuals to form investment funds, tend to purchase companies using debt, with an eye to reselling them in a few years. The industry has turned to health care fairly recently, but it has begun purchasing doctors’ practices at a steady clip, combining smaller practices to form larger companies.When a private equity arm of a Canadian pension fund, OMERS Private Equity, bought Gastro Health, a large gastroenterology medical group, in 2021, it proceeded to acquire nearly a dozen smaller practices, according to the researchers, who say the group is now dominant in markets including the Miami area. The company now operates in seven states, employing over 390 doctors. The researchers saw similar patterns in other markets, where a firm would buy one large practice, then increase its market share by adding nearby smaller practices in the same medical specialty.Historically, doctors’ practices have been relatively small, and owned by doctors themselves. But that model has been rapidly declining as the business of medicine has become more complex and the insurance companies that negotiate with doctors over prices have become bigger. Nearly 70 percent of all doctors were employed by either a hospital or a corporation in 2021, according to a recent analysis from the Physicians Advocacy Institute.“We’re seeing a fundamental change in how medicine is being practiced in the U.S.,” said Richard Scheffler, a professor of health economics and public policy at Berkeley and director of the Petris Center.Hospitals and insurance companies have also bought out many independent physicians’ practices. Optum, an arm of the publicly traded UnitedHealth Group, which also owns one of the nation’s largest insurers, employs roughly 70,000 physicians. Studies have shown that these types of concentrated ownership of doctors in a given market are also associated with higher prices.Private equity is often viewed by physicians as an attractive alternative to having their practice bought by a hospital. In part, the doctors are “getting more scale and gaining efficiencies,” including help with office administration and technology, said Lisa Walkush, a national managing principal for the professional services firm Grant Thornton. “It can be a really good thing, but the private equity firms have to keep their promises and be held accountable,” she said.Michael Kroin, the founder and chief executive of Physician Growth Partners, a Chicago firm that advises independent practices, said the private equity firms “provide scale to allow independent practice groups to survive and maintain their autonomy.” If they could, given their rising costs and how squeezed they feel by insurers, “every independent group would want to increase its fees,” he said.The private equity industry has begun to attract particular scrutiny from researchers and policymakers. Lawmakers in the House are considering legislation to require more reporting when the firms buy health care companies. Currently, the acquisitions can be difficult to track. The authors of the new paper relied on data on deals from a company called PitchBook, which they then matched with doctors in a health care claims database to measure payments from private health insurers.The researchers couldn’t be sure whether the payment increases they measured happened because doctors were performing more complex procedures or just negotiating higher prices, but they suspected the prices explained most of the effect.Previous studies of private equity-acquired hospitals and physician practices from Zirui Song, an associate professor of health policy and medicine at Harvard Medical School, have also documented increasing revenue associated with the purchases. In an interview, Dr. Song said he expected the industry would continue to buy doctors’ practices in the coming years. “We still have a lot of small physician-owned specialty practices,” he said. “That’s an opportunity for consolidation. It’s an easy opportunity.”Critics of the industry, including Professor Scheffler, have also raised concerns about the medical care delivered by private equity-owned health care companies, arguing that the industry’s emphasis on profits could cause patient harm. Research on private equity ownership of nursing homes has shown evidence of lower staffing levels and higher rates of prescriptions for antipsychotic medicines.But little rigorous research has been published on patient care in the office-based medical specialties that the new paper focuses on.How the change in ownership and independence affects doctors and how they treat patients “has been very severely understudied,” said Barak Richman, a professor of law and business administration at Duke University, who reviewed the paper. But he said there is evidence that these firms are skilled at exploiting loopholes in existing regulations to maximize their profits.“Private equity is like the system on steroids,” said Sherry Glied, the dean of the Wagner School of Public Service at New York University. “Every time there’s an opportunity for making money, P.E. is going to move faster than everyone else. And consolidation is the way to do that.”While federal regulators are contemplating changes to how they oversee these deals, researchers say the report underscores the need to pay attention to what happens when a company makes a series of seemingly modest acquisitions. “This builds the case for strong antitrust tools for these incrementally small but collectively larger consolidation trends,” said Erin Fuse Brown, the director of the Center for Law, Health and Society at Georgia State University.
Read more →