Health Risks From Cannabis May Grow as Users Age
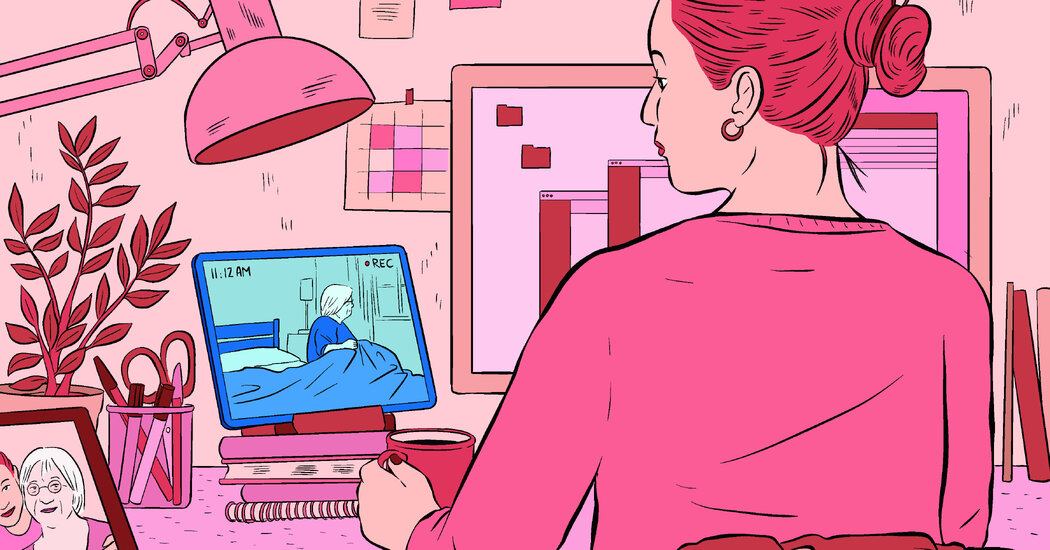
More older people are using cannabis products regularly, but research suggests their cannabis-related health problems are also on the rise.Dr. Benjamin Han, a geriatrician and addiction medicine specialist at the University of California, San Diego, tells his students a cautionary tale about a 76-year-old patient who, like many older people, struggled with insomnia.“She had problems falling asleep, and she’d wake up in the middle of the night,” he said. “So her daughter brought her some sleep gummies” — edible cannabis candies.“She tried a gummy after dinner and waited half an hour,” Dr. Han said.Feeling no effects, she took another gummy, then one more — a total of four over several hours.Dr. Han advises patients who are trying cannabis to “start low; go slow,” beginning with products that contain just 1 or 2.5 milligrams of tetrahydrocannabinol, or THC, the psychoactive ingredient that many cannabis products contain. Each of the four gummies this patient took, however, contained 10 milligrams.The woman started feeling intense anxiety and experiencing heart palpitations. A young person might have shrugged off such symptoms, but this patient had hypertension and the heart arrhythmia called atrial fibrillation. Frightened, she went to an emergency roomLab tests and a cardiac work-up determined that the woman wasn’t having a heart attack, and the staff sent her home. Her only lingering symptom was embarrassment, Dr. Han said. But what if she’d grown dizzy or lightheaded and was hurt in a fall? He said he has had patients injured in falls or while driving after using cannabis. What if the cannabis had interacted with the prescription drugs she took?We are having trouble retrieving the article content.Please enable JavaScript in your browser settings.Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.Thank you for your patience while we verify access.Already a subscriber? Log in.Want all of The Times? Subscribe.
Read more →