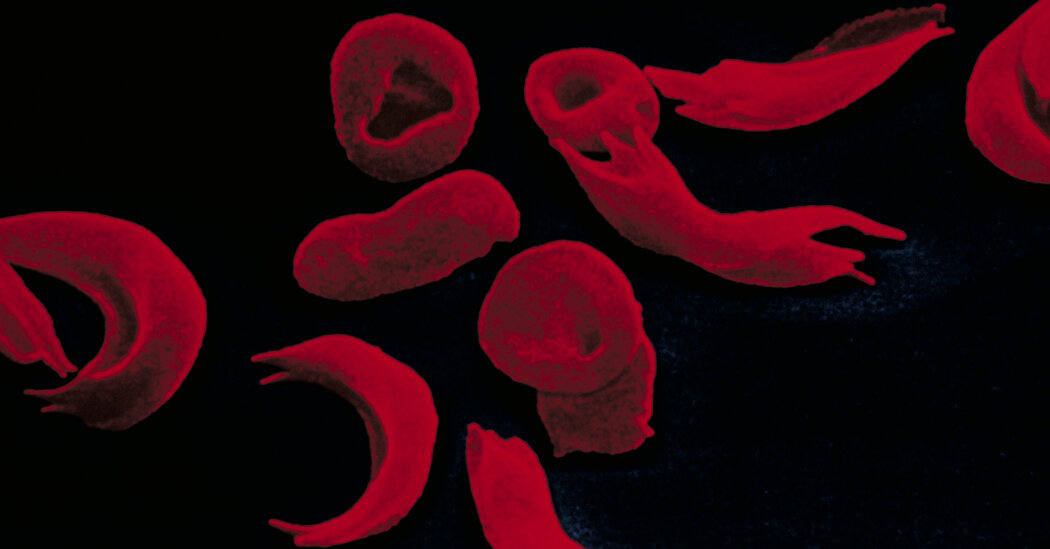
The genetic treatment targeted a particular kind of congenital deafness and will soon be tried in children who are younger.Aissam Dam, an 11-year-old boy, grew up in a world of profound silence. He was born deaf and had never heard anything. While living in a poor community in Morocco, he expressed himself with a sign language he invented and had no schooling.Last year, after moving to Spain, his family took him to a hearing specialist, who made a surprising suggestion: Aissam might be eligible for a clinical trial using gene therapy.On Oct. 4, Aissam was treated at the Children’s Hospital of Philadelphia, becoming the first person to get gene therapy in the United States for congenital deafness. The goal was to provide him with hearing, but the researchers had no idea if the treatment would work or, if it did, how much he would hear.The treatment was a success, introducing a child who had known nothing of sound to a new world.“There’s no sound I don’t like,” Aissam said, with the help of interpreters during an interview last week. “They’re all good.”While hundreds of millions of people in the world live with hearing loss that is defined as disabling, Aissam is among those whose deafness is congenital. His is an extremely rare form, caused by a mutation in a single gene, otoferlin. Otoferlin deafness affects about 200,000 people worldwide.The goal of the gene therapy is to replace the mutated otoferlin gene in patients’ ears with a functional gene.Although it will take years for doctors to sign up many more patients — and younger ones — to further test the therapy, researchers said that success for patients like Aissam could lead to gene therapies that target other forms of congenital deafness.It is a “groundbreaking” study, said Dr. Dylan K. Chan, a pediatric otolaryngologist at the University of California, San Francisco, and director of its Children’s Communication Center; he was not involved in the trial.The one in which Aissam participated is supported by Eli Lilly and a small biotechnology firm it owns, Akouos. Investigators hope to eventually expand the study to six centers across the United States.Special earphones being used for Aissam’s hearing test. His form of deafness is rare, caused by a mutation in a single gene, otoferlin. Hannah Beier for The New York TimesAissam’s trial is one of five that are either underway (the others are in China and Europe) or about to start.Investigators from all five of the studies will be presenting their data on Feb. 3 at a meeting of the Association for Research in Otolaryngology.The studies, researchers said, mark a new frontier for gene therapy which, until now, had steered clear of hearing loss.“There has never been a biological or medical or surgical way to correct the underlying biological changes that cause the inner ear to not function,” Dr. Chan said.Although otoferlin mutations are not the most common cause of congenital deafness, there is a reason so many researchers started with it. That form of congenital deafness, said Dr. John A. Germiller, an otolaryngologist who is leading the CHOP study, is “low hanging fruit.”The mutated otoferlin gene destroys a protein in the inner ear’s hair cells necessary to transmit sound to the brain. With many of the other mutations that cause deafness, hair cells die during infancy or even at the fetal stage. But with otoferlin deafness, hair cells can survive for years, allowing time for the defective gene to be replaced with gene therapy.Aissam’s trial at the Children’s Hospital of Philadelphia is among five that are either underway (the others are in China and Europe) or about to start.Hannah Beier for The New York TimesThere’s an advantage in using gene therapy to allow children to hear. Most of the mutations that affect hearing — there are approximately 150 — do not affect any other part of the body. Some genes are actually unique to the ear.The inner ear is a small closed compartment, so gene therapy delivered there would not affect cells in other parts of the body, said Manny Simons, chief executive and co-founder of Akouos and senior vice president of gene therapy at Lilly.But getting the genes to the cochlea, a spiral-shaped cavity close to the center of the skull, is challenging. The cochlea is filled with fluid, is lined with 3,500 hair cells and is encased in a dense dome of bone with a tiny, round membrane. Sound sets off a wave of fluid in the cochlea and stimulates the hair cells to transmit signals to the brain. Each hair responds to a different frequency, enabling a person to hear the richness of sound.The gene therapy consists of a harmless virus carrying new otoferlin genes in two drops of liquid that are delicately injected down the length of the cochlea, delivering the genes to each hair cell.Yet despite the promise of otoferlin gene therapy, finding the right patients for the trial was difficult.One issue is the very idea of treating deafness.“There is an internal Deaf community that doesn’t see itself as needing to be cured,” said Dr. Robert C. Nutt, a developmental and behavioral pediatrician in Wilmington, N.C., who is deaf.Some Deaf parents, he added, celebrate when their newborn baby’s hearing test indicates that the baby is deaf too and so can be part of their community.Making the issue of gene therapy even more complicated is the standard intervention for otoferlin hearing loss: a cochlear implant. The device, which uses electrodes to stimulate auditory nerves in the inner ear, allows patients to hear sounds, especially those needed to understand speech. But the implant does not provide the full richness of sound — and is said to assist in hearing but without restoring it completely.Dr. John Germiller, an otolaryngologist who is leading the CHOP study.Hannah Beier for The New York TimesMost babies born with otoferlin deafness get cochlear implants in infancy and are therefore ineligible for the trial. The implants somewhat alter the cochlea, which could hamper the interpretation of gene therapy results.The Food and Drug Administration, which allowed the CHOP study to go forward, asked that, for safety reasons, the researchers start with older children, not infants, and treat only one ear.The challenge for the U.S. study was to find older children whose parents would agree to the study, who had otoferlin deafness and who did not have cochlear implants.Aissam never had cochlear implants. He never had schooling in Morocco to help him develop communication skills. But three years ago, when he was 8, his father, Youssef Dam, a construction worker, got a job in Barcelona, Spain. For the first time, Aissam went to school, enrolling in a school for the deaf, where he learned Spanish Sign Language. Soon after, his family learned of the gene therapy trial.When Aissam was deemed eligible to be patient No. 1, Lilly and Akouos paid for him and his father to live in Philadelphia for four months, while Aissam received gene therapy and follow-up hearing tests.No one knew whether the nerve cells that communicate with the hair cells of the cochlea would still be intact and functional in someone who had been deaf for 11 years, Dr. Simons of Lilly said.It was not even clear what dose of the new genes to give. All that the researchers had to go on were studies with mice. “We were flying blind,” Dr. Germiller said.Aissam’s results, his doctors said, were remarkable. In an interview at CHOP, his father said through an interpreter — he speaks a North African language from the Amazigh family, commonly known as Berber — that Aissam was hearing traffic noises just days after the treatment. When Aissam had a hearing test two months later, his hearing in the treated ear was close to normal.But no matter how well the gene therapy works, the researchers recognize that Aissam may never be able to understand or speak a language, Dr. Germiller said. The brain has a narrow window for learning to speak beginning around ages 2 to 3, he explained. After age 5, the window for learning spoken language is permanently shut.Hearing can still help patients even if they never learn to speak, he noted. They can hear traffic or know when someone is trying to communicate. The ability to hear also can help with lip reading.Aissam signing to an interpreter during an interview at the children’s hospital.Hannah Beier for The New York TimesNow that gene therapy has proved safe for Aissam and for another child in Taiwan treated two months after him, researchers at the hospital in Philadelphia are able to move on to younger children. They have two lined up, a 3-year-old boy from Miami and a 3-year-old girl from San Francisco, both of whom got cochlear implants in only one ear, so that the other could be treated with gene therapy.If the Lilly trial of otoferlin gene therapy is proved to be effective and safe, “there will be a lot of interest in other genes” that cause deafness, said Dr. Margaret A. Kenna, an otolaryngologist at Boston Children’s Hospital and professor of otolaryngology at Harvard Medical School.Dr. Kenna, an investigator in the Lilly trial, added, “It’s been a long time coming.”“For decades people have been saying, ‘When is this going to work?’” Dr. Kenna said. “I didn’t think gene therapy would begin in my practice lifetime. But here it is.”Of the other studies, two are in China where investigators are treating younger children and in both ears. Results from one, supported by the National Natural Science Foundation of China and Shanghai Refreshgene Therapeutics, will be reported Wednesday in the journal The Lancet. The other is supported by Otovia Therapeutics and various programs in China.A third study is sponsored by Regeneron and Decibel Therapeutics. Researchers in Europe so far have treated one child, who is younger than 2, and in one ear. Another study by Sensorion is expected to start this month.On a recent frigid morning, Aissam sat in a conference room at CHOP and, with the help of three translators, patiently answered questions about his remarkable experience. He’s a solemn child with a round face and big brown eyes. There was an interpreter for his father, and the sign language team had a Certified Deaf Interpreter — a person who is deaf translated his signs into American Sign Language — and an interpreter who knew American Sign Language and spoke his words.Their system worked to a certain extent but robbed the conversation of spontaneity and forced Aissam to answer in short sentences or phrases, minimizing the expression of his personality.But Aissam managed to convey the wonder of hearing.Noises and voices frightened him initially, he said. But then, as the world of sound opened up, he began to enjoy every sound he heard — elevators, voices, the sound of scissors snipping his hair at a barbershop.And there was music, which he heard for the first time one day while getting his hair cut.Asked if there was a sound he particularly liked, Aissam did not hesitate.“People,” he signed.
Read more →