Thousands of people to trial Alzheimer’s blood tests
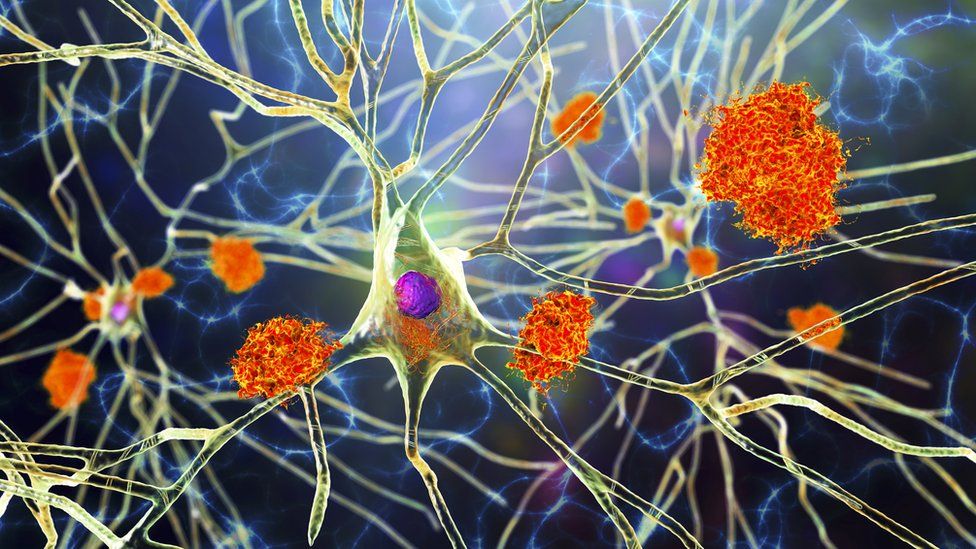
Published9 minutes agoShareclose panelShare pageCopy linkAbout sharingImage source, Getty ImagesBy Fergus WalshMedical editor Memory clinics across the UK are to begin trialling blood tests to see if they can accurately diagnose dementia.The hope is that more people will be able to access care, support and new drug treatments at an earlier stage.The research, by University College London and the University of Oxford, will involve around 5,000 volunteers. The five-year project will study blood tests for Alzheimer’s disease and other forms of dementia.Currently, around a third of patients with dementia never get a formal diagnosis and are left with worry and uncertainty about their condition.Rogue proteinsOnly around 2% of patients have one of the ‘gold standard’ tests for Alzheimer’s – either a specialist PET brain scan or a spinal lumbar puncture.Both can show the presence of rogue proteins in the brain such as amyloid and tau which start to accumulate up to 20 years before symptoms emerge – but tests are expensive. The Oxford team will be looking at a range of blood tests, which could be a cheaper and easier way for doctors to spot early signs of the disease. One blood test will look for traces of these proteins in the blood in order to diagnose Alzheimer’s disease, the most common form of dementia. Some tests will also look for potential biomarkers for vascular and frontotemporal dementia, and dementia with Lewy bodies. The researchers will also look at whether the blood tests can help detect these diseases at various stages.NHS ‘not ready’ for new Alzheimer’s drugsNHS exploring Alzheimer’s disease blood testsHow common is early Alzheimer’s?Dr Vanessa Raymont, from the University of Oxford, is leading a study which will recruit volunteers from more than 50 UK trial sites, which are all NHS memory clinics. She told the BBC that although several dementia blood tests had already shown promising results, they had limitations. “Research has tended to exclude the very elderly, ethnic minorities and those with other medical conditions so we need to understand what the data looks like in the real world, which is why these projects are so important.”The University College London (UCL) team will focus on the most promising biomarker for Alzheimer’s disease, called p-tau217, which can indicate levels of amyloid and tau in the brain.Its trial will see if measuring p-tau217 in the blood can increase the rate of diagnosis for Alzheimer’s disease in people with early dementia, but also those with mild but progressive memory problems.Access to new treatmentsJonathan Schott, professor of neurology at UCL, who is leading the trial, said: “An early, accurate diagnosis of Alzheimer’s disease is already important, allowing people to access appropriate care and medications. “If, as we hope, new treatments that can slow down Alzheimer’s disease become available soon, then this will be vital,” he said.”This would pave the way for fair and equitable access to new and potentially life-changing treatments to all who might benefit.”Two treatments have shown in trials that they can slow the progression of early stage Alzheimer’s. Doctors say the benefits are modest but they represent the first ‘disease-modifying’ drugs. The drugs, lecanemab and donanemab, are currently being considered by the MHRA, the body which approves drugs in the UK. Even if they are granted licences, they would then need to be given the green light by health assessment bodies which consider their cost-effectiveness for the NHS, before being rolled out to patients. Dr Sheona Scales, director of research at Alzheimer’s Research UK, said: “We’ve seen the enormous potential that blood tests are showing for improving the diagnostic process for people and their loved ones in other disease areas.”She said it was important to see “the same step-change in dementia”, which is the greatest health challenge facing the UK.The Blood Biomarker Challenge is being funded by Alzheimer’s Society, Alzheimer’s Research UK, the National Institute for Health and Research and Gates Ventures, including £5m from People’s Postcode Lottery.More on this storyNHS ‘not ready’ for new Alzheimer’s drugsPublished12 FebruaryNHS exploring Alzheimer’s disease blood testsPublished9 November 2023New drugs for Alzheimer’s hailed as turning pointPublished17 July 2023Fiona Phillips: How common is early Alzheimer’s?Published5 July 2023Blood test for early Alzheimer’s ‘shows promise’Published29 July 2020First drug that can slow Alzheimer’s dementiaPublished22 October 2019Lifestyle changes that could lower your dementia riskPublished14 July 2019
Read more →