New Parkinson’s drug to be rolled out on NHS
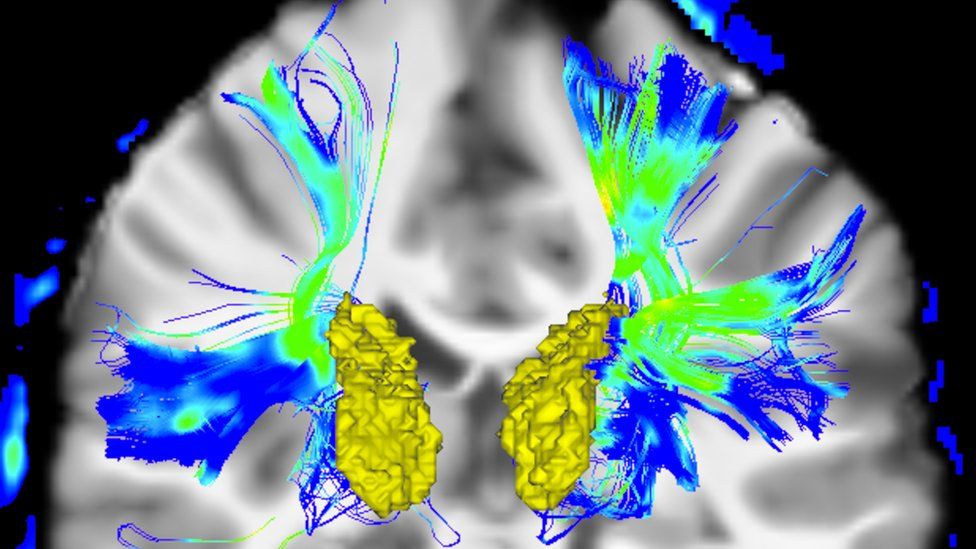
Published20 minutes agoShareclose panelShare pageCopy linkAbout sharingImage source, Getty ImagesBy Aurelia FosterHealth reporterNearly 1,000 people with advanced Parkinson’s disease are to benefit from a new treatment that involves wearing a portable kit 24 hours day.NHS England is to roll out the treatment, Produodopa, which uses a pump to steadily release medicine into the bloodstream round the clock.Many people currently need to take more than 20 pills a day to control their symptoms – with an inconsistent effect.Others have to be treated through a permanent feeding tube. Produodopa is a combination of two drugs – foslevodopa and foscarbidopa. It works by turning foslevodopa into the chemical dopamine, which helps transmit messages between the parts of the brain and nerves that control movement.That helps manage Parkinson’s symptoms, such as excessive movement or tremors.The infusion enters the patient’s bloodstream through a cannula under the skin and is controlled by a small, automatic pump, releasing a steady flow of the treatment 24 hours a day to stay on top of symptoms. It also has the option of a manual boost if needed.Many patients currently taking a large number of tablets to control their symptoms say they worsen later in the day and during the night.Parkinson’s implant restores man’s ability to walkTai Chi may slow Parkinson’s symptoms by years – studyCould Parkinson’s could be detected early with AI scans?James Palmer, NHS England’s medical director for specialised services, said the drug’s rollout was “great news”.”This important therapy will now offer a vital new option on the NHS for those who aren’t suitable for other treatments such as deep brain stimulation,” he said. “We hope it will help nearly 1,000 patients to manage their symptoms more effectively and go about their day with a better quality of life.”The drug has recently been approved for NHS use by the National Institute for Health and Care Excellence, after successful clinical trials.Image source, NHS EnglandJohn Whipps, 70, took part in the research and says his life is much more “plan-able” now that he is on the new treatment.”Before this, I was on nearly 20 tablets a day just for my Parkinson’s symptom control, and then all the other tablets on top of that,” he said.”And I would frequently wake in the middle of the night with internal tremors and take more tablets, but this pump just keeps running through the night.”I couldn’t plan to do anything, as you don’t know if you’re going to have an off day and need to stay at home.”Another participant in the trial, Phil, 52, from Cornwall, said he previously had to take 25 tablets daily and his symptoms fluctuated through the day, becoming worse at night.”At night, I was normally not able to turn over in bed, or get up for the toilet, and if I did manage it, I was at risk of falls,” he said.”Whilst wearing the pump, it delivered the drug whilst I was sleeping, enabling me to turn over at night, and get up for the toilet which made a huge difference at night.”It is hoped the new treatment will also some benefit patients who currently receive drugs through a permanently placed feeding tube into the gut.Parkinson’s disease, a condition in which parts of the brain become progressively damaged over many years, affects around 128,000 people in England, according the NHS.Parkinson’s UK describe it as “the fastest growing neurological condition in the world”.Laura Cockram, from the charity, said Produodopa could be a “life-changing option” for some people.”It won’t be suitable for everybody though, and people with Parkinson’s should speak to their consultant or Parkinson’s nurse to see whether it’s an option for them,” she added. More on this storyPesticide maker used ‘weak’ data on Parkinson’sPublished3 days agoParkinson’s implant restores man’s ability to walkPublished6 November 2023Tai chi may slow Parkinson’s symptoms, study findsPublished25 October 2023AI scans could detect Parkinson’s, scientists sayPublished22 August 2023Blood test spots Parkinson’s risk before symptomsPublished7 December 2023’There is life after Parkinson’s diagnosis’Published8 December 2023Related Internet LinksHomepage – Parkinson’s UKNHS EnglandNICE – The National Institute for Health and Care ExcellenceThe BBC is not responsible for the content of external sites.
Read more →