Abortion Insurance Coverage Is Now Much More Complicated
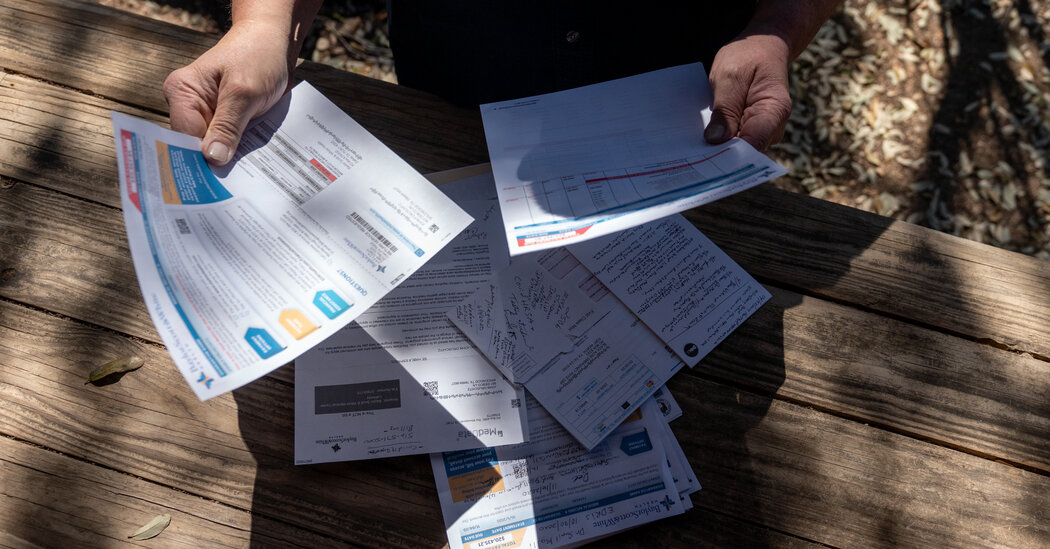
In the wake of the Supreme Court ruling, abortion benefits will depend even more on where a woman lives and who provides her insurance.Even before the constitutional right to an abortion was struck down last month, health insurance coverage for it was spotty. Abortion benefits largely depended on where a woman lived or whom she worked for.Those factors have become even more crucial now that the Supreme Court has left it to the states to regulate abortion. The existing patchwork of coverage is likely to become more restrictive, and the gulf will widen between states that had already banned abortion-related benefits and those that mandate coverage.Dozens of large employers are attempting to fill the gaps by paying expenses for workers who need to cross state lines for a legal abortion, though there are still questions about how much risk companies are taking on and how far an anti-abortion state — or an aggressive prosecutor — could go to stop them.For women without that extra support or coverage, the new logistical challenges and the added costs may be impossible to overcome.“People with financial resources will find ways to get the treatment they want or need,” said Susan M. Nash, a benefits lawyer and partner at Winston & Strawn with expertise in health care. “But the people who can’t travel or have limited means to access treatment outside of the health plan will be adversely impacted here.”Here’s a look at how the decision, Dobbs v. Jackson, may affect insurance coverage across the country:How much does an abortion cost?The median cost to a patient for a medication abortion — which involves two drugs, generally taken up to 10 to 12 weeks of pregnancy — was $560 in 2020, according to a recent study at the University of California San Francisco’s Advancing New Standards in Reproductive Health program. A procedural abortion was $575 during the first trimester and $895 during the second trimester. That doesn’t include travel costs and other expenses, such as child care and time off from work, which will be increasingly necessary for women in a growing number of states. And costs varied substantially by region.Most patients pay out of pocket, research has found, in large part because their insurance doesn’t cover the procedure. Even before the Dobbs decision, 11 states restricted the type of abortion coverage private health insurance plans could cover, and 26 states barred all plans in their state’s health insurance exchange from covering abortion, researchers found.“The people who can’t travel or have limited means to access treatment outside of the health plan will be adversely impacted here,” said Susan M. Nash, a benefits lawyer.Callaghan O’Hare for The New York TimesWill Medicaid cover abortion?Just like before the ruling, that largely depends on where you live.Medicaid, a public health program largely for low-income households that is administered by the states, is financed by federal and state money. Even before the Dobbs decision, federal law — known as the Hyde Amendment — didn’t allow federal funds to pay for abortions, except in limited circumstances: if the pregnancy was the result of rape or incest or caused a life-endangering condition for the woman. States could choose to use their own money to pay for abortions beyond those situations, and 16 states had such policies last year, according to the Kaiser Family Foundation (though nine were ordered by courts to have them).The vast majority of states don’t pay for anything beyond those limited circumstances — and South Dakota, in violation of federal law, covers abortions only in the case of life endangerment, according to a 2019 study by the Government Accountability Office.Read More on the End of Roe v. WadeA Culture Warrior Goes Quiet: Gov. Ron DeSantis of Florida celebrated the end of Roe. But his hesitance to detail his plans for abortion policy in his state reflects the new and difficult political terrain for Republicans.Under Pressure to Act: Democrats in Congress are moving ahead on measures to preserve abortion access, but with Republicans and at least one Democrat opposed in the Senate, the bills are all but certain to fail.The Right to Travel?: Justice Brett M. Kavanaugh said the Constitution did not allow states to stop women from traveling to get abortions. But what a state may choose to do if a resident travels to get an abortion is not clear.‘Pro-Life Generation’: Many young women mourned the Supreme Court decision to overturn Roe. For others it was a moment of triumph and a matter of human rights.Like South Dakota, a growing list of states that ban abortions — including Alabama, Arkansas, Louisiana and Missouri — make exceptions only when the woman’s life is endangered. That puts them in conflict with federal law that also requires abortion coverage in cases of rape or incest.The Centers for Medicare & Medicaid Services said it would notify states when they were out of compliance with federal requirements, and added that the Department of Health and Human Services was taking steps to expand access to medication abortion in those limited circumstances. Details on how that will happen are still vague.What about marketplace plans?The health insurance marketplace created under the Affordable Care Act has similar restrictions. Plans offered within the marketplace are not required to cover abortion, and federal money — including premium subsidies in the form of tax credits — cannot be used to pay for them. Here, too, there are exceptions for rape, incest and life endangerment, but they are not universal.There are 26 states that ban marketplace plan coverage of abortions, said Alina Salganicoff, director of women’s health policy at Kaiser. But a few states don’t make exceptions for rape or incest, and some states make no exceptions at all, she added.In contrast, insurers in seven states are required to include abortion coverage in all plans sold on the marketplace, according to Kaiser, but no federal dollars are used.For example, in states like New York, where abortion is legal under state law, policy holders with subsidized marketplace plans have $1 of their monthly premium held separately to be used for abortion and other services.But if an individual with a marketplace plan lives in a state where abortion is banned, it’s likely their policy won’t provide coverage in their own state or across state lines.Abortion rights protesters at the Utah State Capitol in Salt Lake City after the Supreme Court overturned Roe v. Wade last month.Kim Raff for The New York TimesI’m covered by my employer’s plan. Will my benefits change?That will depend on where you live, the type of insurance plan your employer uses and their stance on coverage.Basically, if a company pays for its employees’ health care from its own coffers, workers, even those in states where abortion is illegal, may have broader access to benefits. But employers that buy insurance policies for workers could be further restricted.Large employers are often self-insured, which means they collect a share of their workers’ premiums and pay for their health care (though an insurer or administrator usually processes claims). These plans generally follow federal rules under the Employee Retirement Income Security Act of 1974, known as ERISA, which provide broad flexibility in designing a health care plan.Other employers buy insurance on behalf of their workers, and the insurer is responsible for costs. Health insurers are regulated by the states and must follow their rules — if abortion is banned there, you’re unlikely to receive any coverage, even if you travel out of state. Many larger employers are providing travel benefits for workers who would need to cross state lines for abortion. This is often an extension of existing policies. Typically these plans have offered travel benefits for people seeking cancer treatments, transplants or other specialized therapies if they don’t have access to a provider in their state or have to travel a certain number of miles to reach one, benefits lawyers said.But there are still concerns about employers’ criminal and civil liability, particularly in states with laws that would call for criminal prosecution of anyone in the state who “aids and abets” an abortion, even if it occurs in another state where abortion is legal.Health plans governed by federal ERISA regulations may have additional protections against legal actions brought under state law, benefits experts said, as long as the services are legal in the state where they are provided. Benefits lawyers also point to Justice Brett Kavanaugh’s concurrence in Dobbs, in which he said states with abortion bans could not stop women from seeking the procedure elsewhere. But while ERISA regulations often supersede state laws that may apply to plans, that doesn’t extend to state criminal laws.“This issue will likely be the subject of continuing litigation and debate,” according to the reproductive rights task force at Morgan Lewis, a law firm in Washington.Traveling to another state for an abortion raises a host of unanswered questions. “If there is a criminal statute in the state you live in, you need to be concerned,” said Amy M. Gordon, a lawyer.Jamie Kelter Davis for The New York TimesWill my employer coverage work differently if I travel out of state?That depends on your plan.But when an insured person travels out of state for an abortion or related medication, it’s more likely the providers will fall outside the plan’s network, which generally costs the insured person more or means expenses will be reimbursed at a lower rate, said Sarah Raaii, a senior associate at McDermott, Will & Emery. Some employers could decide to ease that burden by making up the difference and covering certain out-of-network procedures and services at the in-network rate, she added.What does the ruling mean for telehealth coverage?Women in states with abortion bans may consider getting prescriptions for abortion-related drugs through a telehealth visit from a provider located in a state where abortion is permitted.It may not be easy. Even before the Dobbs decision, some states banned telehealth visits from prescribing abortion-inducing medications or had other rules that limited the feasibility of remote visits anyway. And six states had laws that banned the mailing of abortion drugs, according to Kaiser.With broader abortion bans, the rules around telehealth visits and insurance coverage may become trickier. But one aspect is relatively clear: The location of the patient during the telehealth visit will determine whether it’s legal to prescribe abortion medication at that time, said Marshall E. Jackson Jr., a partner with McDermott Will & Emery who focuses on digital health care.For example, a patient living in Missouri, where abortion is banned, could not have abortion medication prescribed during a telehealth consultation while she was in her home state. But if the telehealth visit occurred while she was working from her employer’s office in Illinois — and the medication was mailed there — that would be generally permitted, he said.How much do I have to worry about privacy if I use insurance? That will also depend on your location.“If there is a criminal statute in the state you live in, you need to be concerned,” said Amy M. Gordon, a partner and benefits lawyer at Winston & Strawn. “It depends on how aggressive prosecutors will be prosecuting those outside of their state. Therefore, the risks are still open questions.”Let’s say you live in a state where abortion is banned but you travel to another state to receive a prescription for abortion-inducing drugs or to have the procedure. When plan benefits are used to pay, that information is generally protected under the Health Insurance Portability and Accountability Act, known as HIPAA, the federal rule that governs the privacy of a patient’s health records.But medical and billing records that are typically kept private can be released without the patient’s written permission in response to a warrant or subpoena.“An employer that sponsors a group health plan can argue this is protected health information, and therefore it should not be turned over,” Ms. Gordon said. “However, this is not bulletproof. There are provisions in HIPAA that permit disclosure to law enforcement seeking to enforce the law.”There are now questions about whether traveling out of state for an abortion will be covered by insurance plans.Anna Rose Layden for The New York TimesAre there resources for people without insurance?Yes. The federal government is encouraging people to visit reproductiverights.gov, which includes links to other resources that can help users find abortion providers and so-called abortion funds, which can provide financial assistance.According to the Guttmacher Institute, a reproductive health research group that supports abortion rights, there are more than 80 abortion funds that help patients seeking the procedure or medication. Other groups, including the Brigid Alliance, help provide travel, lodging and logistical support to patients.Is coverage for infertility treatments or contraceptives affected?Contraceptive coverage is not affected by the ruling. Most private health plans, including plans in the health insurance marketplace, must cover contraceptive methods and counseling, including emergency contraceptives, as prescribed by a health care provider, according to Ellen Montz, director of the Center for Consumer Information and Insurance Oversight at the Center for Medicare & Medicaid Services.These plans must cover these services without charging a co-payment or coinsurance when provided by an in-network provider — even if someone hasn’t met the deductible, she added.But there are fears that some types of infertility treatments, which are increasingly covered by employer-provided insurance, could be restricted, depending on the legal language included in abortion bans.Legal experts say new rules don’t pose an immediate threat to infertility patients, their health care providers and embryos created in labs, but that could quickly change, depending on how the new abortion bans are enforced.“That could be the next frontier,” said Ms. Raaii of McDermott, Will & Emery, “through which states try to enforce these laws against patients, providers, employers, payers or others.”
Read more →